Hoping To Cure Blindness, Scientists Develop ‘Mini Retinas’ From Stem Cells: The Power Of Organoids
In the past five years, a new form of stem cell research has surfaced. Instead of focusing on creating full organs from pluripotent stem cells, it involves building organoids — complex 3D organ tissues in lab dishes that aren’t quite organs yet — which provide clearer insight into cell development and diseases.
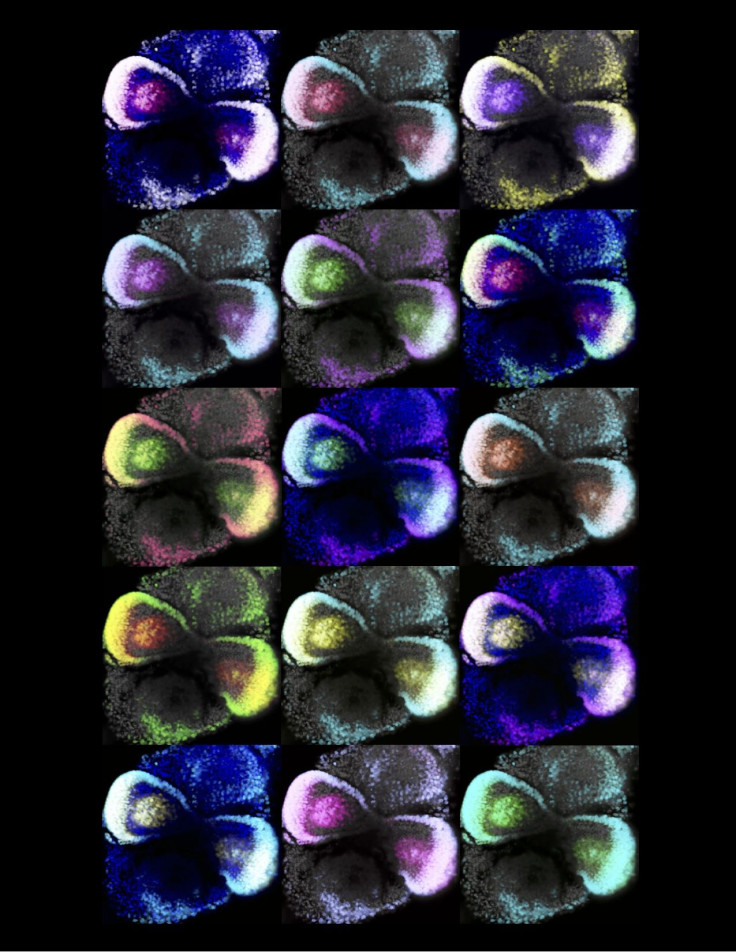
In a small lab in Dresden, Germany, a group of researchers led by Dr. Mike Karl have made a significant step forward in organoid research: They’ve found an effective way to build mini retinas, or retinal organoids, to study eye development and various eye diseases that cause blindness. Their study, published in Stem Cell Reports, describes the “plasticity of pluripotent stem cells” that “provides new possibilities for studying development, degeneration, and regeneration” of retinal cells, they wrote.
In other words, they induced stem cells to form into mini retinas, which will allow them to study developmental retinal diseases, like age-related macular degeneration, genetic disorders, or eye injuries. “We will use [this method] to develop experimental models — like tearing of the retina, which can happen in young patients, or in older patients when the retina gets thinner,” Karl told Medical Daily. “The biggest goal is to study disease processes,” and ultimately use the technology to study new therapies for the eye.
Little Faces
Mike Karl has been working at the German Center for Neurodegenerative Diseases for five years, focusing primarily on the link between brain plasticity and retinal development and disease. Meeting me on a warm spring day in Dresden, he showed me around his lab; the room where all the mini retinas are created is tiny. They sit quietly in petri dishes, stored away on shelves in cell culture incubators, where they develop at 98.6 degrees Fahrenheit. Mouse retinal organoids take some 20 to 30 days to develop, while human organoids take much longer — up to 180 days, or almost six months.
Much of organoid research is a waiting game. Karl and first author Manuela Völkner explained with cheery patience that we still don’t quite understand what happens when pluripotent stem cells, cells capable of growing into any type of cell in the body, self-regulate into specific cell types. Scientists can create environments with growth factors that nudge the stem cells in a certain direction, but most of the time there’s really no telling what they’ll end up as.
Their new protocol allows them to push cells in the direction of retinal development, but there’s still a big area of flexibility between the nascence of pluripotent stem cells and their last stage. “We are still sitting on the sidelines watching as the power of these pluripotent cells do their thing,” Karl notes.
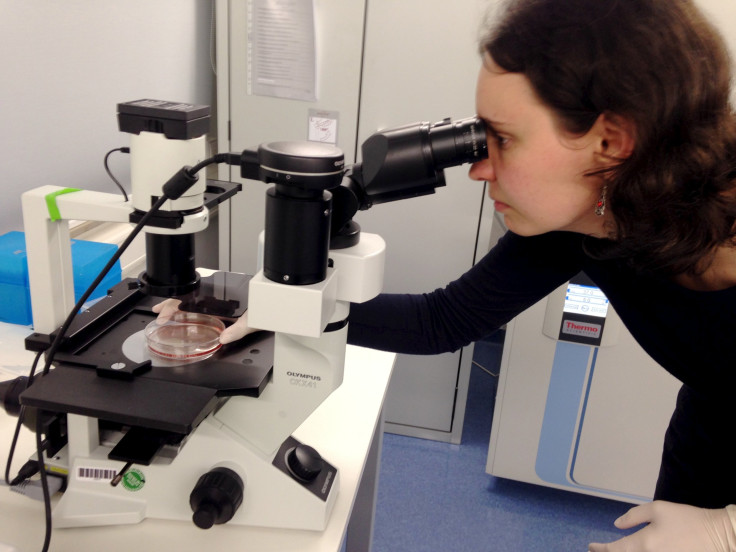
However, they’ve still succeeded in nudging many stem cells to their organoid final stage. Karl’s assistant brought me over to a microscope, and placed a petri dish under it. She let me peer into the dish, which contained retinal organoids in their final stage — two tiny “eye cups” facing one another on either side of the dish. Karl calls them “little faces,” frameworks of the beginning of eyes.
The Power Of The Organoid
These aren’t the first organoids to be developed: Scientists have succeeded in creating protocols for kidney, intestines, and brain organoids. Though the “boom” in organoid research has occurred in the last five years or so, its advent can be traced back to 2008, when Japanese researcher Yoshiki Sasai of the RIKEN Institute in Japan showed that stem cells could be pushed into small clumps of neural cells that self-organized into layers and the beginning of tissues.
Later, in 2013, researchers in Austria developed “mini brain” models from mouse embryonic stem cells. The researchers explained that these organoids weren’t “brains in a jar,” but rather “the very first steps of embryonic brain development, like in the first nine weeks of pregnancy,” Jürgen Knoblich, lead author of that study, told The Scientist. “They’re nowhere near an adult human brain and they don’t form anything that resembles a neuronal network.” However, these “cerebral organoids” allow scientists to study brain diseases in development, which could never be done before in the same way.
The process is similar when it comes to developing retinal organoids. Building from these previous studies, Karl and his team were able to create a method that, for the first time, allowed them to grow complex retinal tissue. Previously, scientists were only able to develop clumps of retinal cells, and couldn’t go much further.
Contrary to popular belief, however, Karl’s main goal isn’t to build a full retina or a full eye from stem cells. His interest lies in investigating the different genetic, age-related, environmental, or traumatic diseases of the retina. “The goal isn’t just to make the closest thing next to a real retina, but also to possibly harness the flexibility of the system to create more diverse ways of studying retina tissue,” Karl said in a press release.
Many of these diseases are linked to scarring of the retinal tissue, but researchers still don’t know exactly why. Studying their development in these organoids would give them the chance to observe disease processes in a way that simply can’t be done in humans. “In [human] patients, you can’t really study the pathology of diseases,” Karl said, mainly because by the time doctors view the symptoms of an eye disorder, it has already been incubating and developing for months or even years. Organoids would allow them to see the disease happen in real-time, from start to finish.
Perhaps most interestingly, at the end of the day, Karl’s research falls under the umbrella of brain plasticity — the focus at the German Center for Neurodegenerative Disease, Germany’s only research institute devoted to studying all dementias and brain degeneration and regeneration. The Dresden center, in particular, focuses on stem cell research and regenerative medicine and how it relates to the brain’s ability to change over time. The ultimate goal at Karl’s lab is to see if they can find ways to regenerate retinal tissues with stem cells, but first, the team plans to expand the organoid protocol into human cells and “carry it much deeper into the human system.” This, Karl said, will pave the way for new therapies.
Source: Völkner M, Karl M, Zschätzsch M, Rostovskaya M, Overall R, Busskamp V. Retinal Organoids from Pluripotent Stem Cells Efficiently Recapitulate Retinogenesis. Stem Cell Reports , 2016.



























