Brain Surgery Through Cheek: New Epilepsy Procedure Sees Point Of Entry Through Patient’s Face
Epilepsy patients could one day see less invasive forms of brain surgery if new research from Vanderbilt University, which looks into using patients’ cheeks as the point of entry to their brains, can reach widespread use.
The current standard for peering into epileptic patients’ brains is to drill straight through their skulls and destroy the guilty tissue. But the area doctors want to look at — the hippocampus — sits in the back of the brain, toward the bottom. Five years ago, this led the researchers to wonder: Is there a better way?
Epilepsy is a neurological disorder, which arises when neurons in separate parts of the brain, and which normally fire at different times, begin firing in synchrony. What results is a seizure, and they’re normally treated with medication. Failing that, doctors will turn to full-on removal. They’ll cut out the misbehaving areas of the hippocampus via the temporal lobe and perhaps even take a part of the neocortex, too. This method helps quiet seizures roughly 60 to 70 percent of the time, although recovery times can be long.
The eureka moment arrived, as they always do, at random. “The idea for this came about when Eric and I were talking in the hallway one day and we figured that his expertise in pneumatics was perfect for the MRI environment and could be combined with the steerable needles I'd been working on,” said Robert Webster, associate professor of mechanical engineering, referring to his colleague Eric Barth.
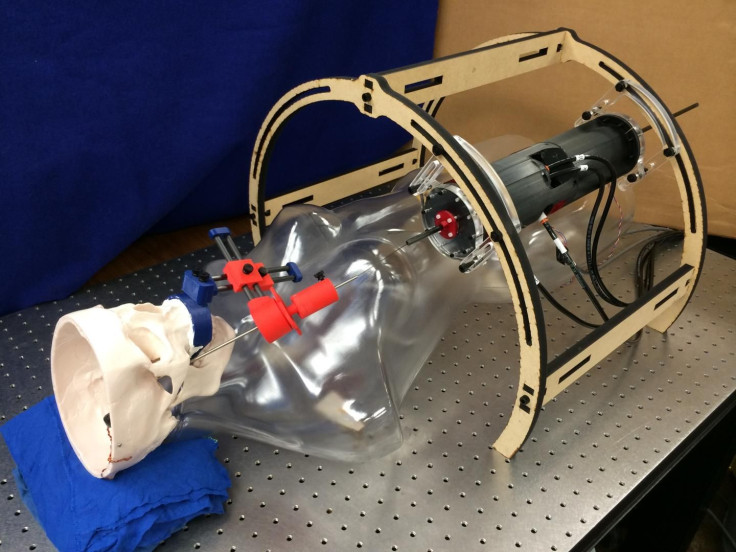
After years of tinkering with different metals and the logistics of entering the brain through a patient’s mouth, the team of engineers and neurosurgeons landed on a nickel-titanium needle whose tip measures 1.14 millimeters in length. It works like a mechanical pencil: As surgeons advance deeper into the tissue, the needle pokes through concentric tubes and curves along a path toward the brain.
This application is new, but the approach isn’t. Neuroscientists already make frequent use of the through-the-cheek approach to implant electrodes in patients’ brains, so that they can track brain activity without whipping out the power tools. But getting rid of the offending tissues demands specificity, and straight needles don’t get the job done.
“The systems we have now that let us introduce probes into the brain — they deal with straight lines and are only manually guided,” said Associate Professor of Neurological Surgery Joseph Neimat. “To have a system with a curved needle and unlimited access would make surgeries minimally invasive.”
Up next for the Vanderbilt team is testing their robot on cadavers. Assuming the device is able to remove the desired patch of tissue, they’ll stick to the timeline that sees the robot entering operating rooms within the decade. To keep costs low, most of the machine’s parts were designed to be made by 3D printers, the team says.



























