Brain Tumors Manipulate The Blood-Brain Barrier In Order To Spread; New Findings Offer Insights For Drug Development
A huge part of stopping cancer and finding new treatments comes from understanding metastasis, or the way cancer spreads through the body. It’s undoubtedly complex, occurring in different ways in different parts of the body. Studies have shown everything from cancer cells following healthier ones as they try to escape to the protein Rac1 becoming more active in cancer cells, helping them to spread. A new study now brings to light how metastasis occurs with the brain cancer glioblastoma.
Metastatic cancers are cancers that have spread from their primary site (where the tumor is) to other parts of the body. The blood vessels and lymph system — vessels that carry fluid and immune system cells — provide highways within the body for the cancer cells to spread efficiently. Glioblastomas are some of the fastest growing tumors in the body because their cells reproduce quickly and the blood vessels within the head provide support for metastasis.
The new study, from researchers at the National Institute of Neurological Disorders and Stroke (NINDS), found that glioblastoma cells are able to bypass several protective mechanisms in the head’s blood-brain barrier (BBB) in order to spread.
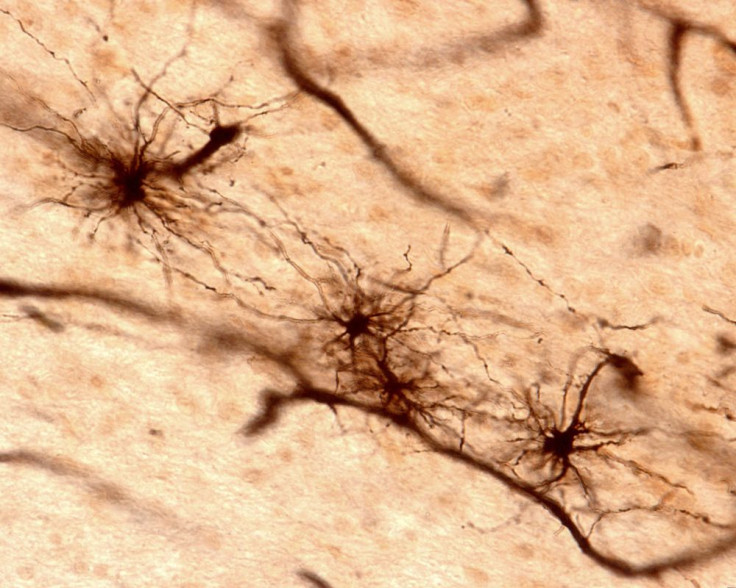
The BBB usually works to protect harmful materials, like chemicals and pathogens, from entering the brain. It works as both a barrier and a regulator of these chemicals with the help of several mechanisms. One of them, called tight junctions, are a set of tight connections between the blood vessels’ endothelial cells. They form an impermeable seal in order to limit diffusion. Astrocytes, another cell that resides in the blood vessels, contain 50 to 60 branching protrusions with “endfeet” at their tips. These endfeet cover 90 percent of the brain’s blood vessel surfaces and release chemicals that regulate the tight junctions as well as the expanding and contracting of the blood vessels.
Using mice, fluorescent dyes, and several brain imaging techniques, the researchers were able to see how glioblastoma spread within the brain. They found that glioblastoma cells outside of the main tumor were sneakily located between the astrocytes and the outer surface of the blood vessel. By doing this, they were able to displace the astrocytic endfeet from the blood vessels and tap into the blood supply for sustenance. This resulted in the loosening of tight junctions, and the eventual breakdown of the BBB.
Historically, treating brain tumors has been difficult due to the protection the BBB provides. But the new research suggests that some drugs could possibly make contact with the tumor cells. “Evidence from our models suggests that early in the disease, invading tumor cells are not completely protected by the blood-brain barrier and may be more vulnerable to drugs delivered to the brain via blood,” said Dr. Harald Sontheimer, of the University of Alabama, Birmingham, in a press release. “If these findings hold true in humans, treatment with anti-invasive agents might be beneficial in newly diagnosed glioblastoma patients.”
More research will be needed before any kind of drugs can begin to be developed. But the findings offer new insight into possible treatments for glioblastomas, which kills most people diagnosed with it within 15 months.
Source: Watkins S, Robel S, Kimbrough I, et al. Disruption of astrocyte–vascular coupling and the blood–brain barrier by invading glioma cells. Nature Communications. 2014.



























