Can Deep Brain Stimulation Treat Obesity? DBS Studied As Last-Ditch Effort In Weight Loss
Food cravings are a mental matter, so why not treat them as such? Researchers have begun studying the effects of deep brain stimulation (DBS) in treating obese and overweight patients based on their metabolic rates and appetites.
The preliminary study involved three people over the course of three years. None reported serious side effects, and two even lost weight temporarily.
Lead researcher of the study and vice chairman of neurosurgery at Allegheny Hospital in Pittsburgh, Dr. Donald Whiting said safety tests precede everything.
"The first thing we needed to do was to see if this is safe," he said. "We're at the point now where it looks like it is."
Whiting conceded that the study was not intended to test the treatment's effectiveness, but rather to open doors of possibility in continuing the research into weight loss alternatives.
"Nobody should get the idea that this has been shown to be effective," Whiting said. "This is not something you can go ask your doctor about."
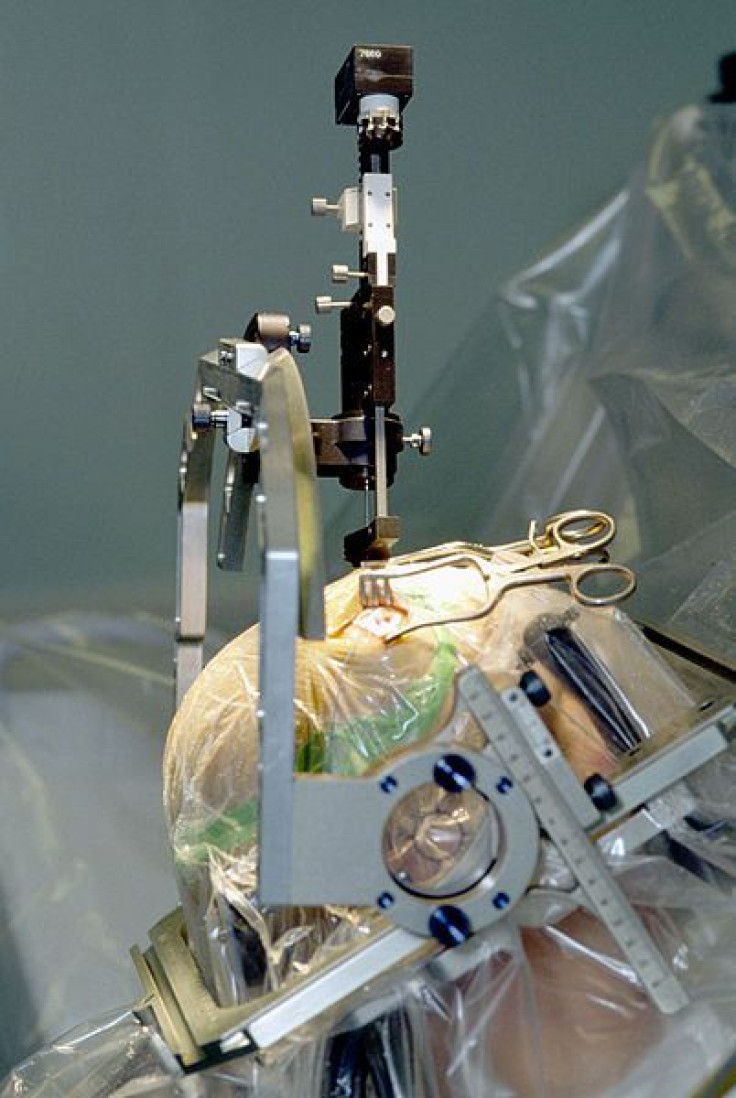
DBS has been used in the past to treat a medley of neurological disorders. The process includes three main parts: the implanted pulse generator (IPG), the lead, and the extension. A doctor implants the IPG into the patient's skin, usually beneath the collarbone or abdomen, and runs an electronic pulse through the extension and into the lead, delivering a disruptive pulse to the afflicting part of the brain. In patients with Parkinson's disease, for instance, doctors tend to disrupt either the subthalamic nucleus (STN) or the globus pallidus interna (GPi).
Whiting's study examined the effect of DBS on appetite, feelings of fullness, and metabolic rates, by targeting the lateral hypothalamic area, similar to previous studies that tested the same area in animals.
Dr. Casey Halpern, a neurosurgeon at the University of Pennsylvania, who was not involved with the study, said Whiting's study makes for interesting and necessary opportunities in the field of DBS.
"Obesity is a major problem," Halpern said, "and current therapies, even gastric bypass surgery, don't always work. There is a medical need for new therapies."
Whiting's patients responded in positive and negative ways to the therapy. Despite reporting short-lived feelings of nausea, anxiety, and feeling "too hot or flushed," the patients also saw intermittent spikes in resting metabolisms as well as temporary weight loss — 12 to 16 percent of their initial body weight.
Short-term weight loss has Whiting curious about what could produce long-term, sustained weight loss. He and his team continue to monitor the patients.
And while DBS seems promising on its face, Whiting advised against people turning to the treatment before exhausting all other possibilities, even gastric bypass surgery, at least in the beginning.
Dr. Halpern added, "At first, it would absolutely be a last-ditch option." However, science cannot rule out the chance of it becoming an add-on therapy — used after gastric bypass or in its place if the surgery is too risky, he said.
Source: Whiting D, Nestor D, Tomycs MD, Bails J. Lateral Hypothalamic Area Deep Brain Stimulation For Refractory Obesity: A Pilot Study With Preliminary Data On Safety, Body Weight, And Energy Metabolism. Journal of Neurosurgery. 2013.



























