Chronic Pain Patients Show Patterns Of Brain Inflammation, Setting Stage For Objective Pain Scale
“On a scale of 1 to 10, how bad is the pain?”
That question has been asked in a variety of settings for an equally colorful range of afflictions. That’s because doctors, despite 76 million Americans having had suffered from chronic pain at one point or another, don’t yet have a standardized scale for measuring pain — after all, what registers as a 6 for you may be a 9 for someone with a lower threshold. Now, a new study finds that a standardized scale may be within reach, and neuroinflammation, of all things, is here to help.
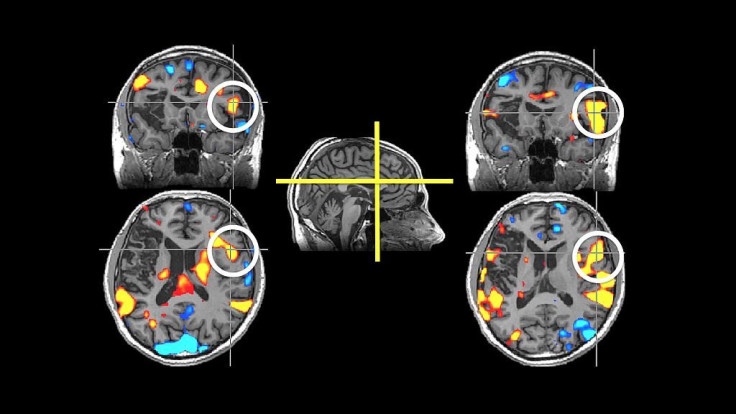
Researchers from Massachusetts General Hospital collected data on 44 subjects, 19 with chronic lower back pain and 25 who were pain-free. Specifically, they performed scans on the brain’s thalamus, a region that, among other things, is responsible for signaling pain. Using a drug that shows up in contrast on the scan when it binds with a particular protein — known as a translocator protein (TSPO) — they could see how chronic pain correlates to inflammation in the brain, which the protein illuminates in the thalamus.
The findings are significant because they offer a future of health care that doesn’t have to rely on questionable data. Unlike physicians, who can look at high blood pressure and cholesterol levels to assess a patient’s risk for disease, people who study pain have had to trust murky self-reports to go in one direction or another. Now, the findings suggest a new approach, in which doctors can enjoy a solid footing for making complex decisions about pain — all from a helpful batch of brain cells.
“Demonstrating glial activation in chronic pain suggests that these cells may be a therapeutic target, and the consistency with which we found glial activation in chronic pain patients suggests that our results may be an important step toward developing biomarkers for pain conditions,” said Marco Loggia, of the MGH-based Martinos Center for Biomedical Imaging, in a statement. The inflammation was so starkly evident in the scans that Loggia could pick apart the control group from the pain group just by looking at them, he added.
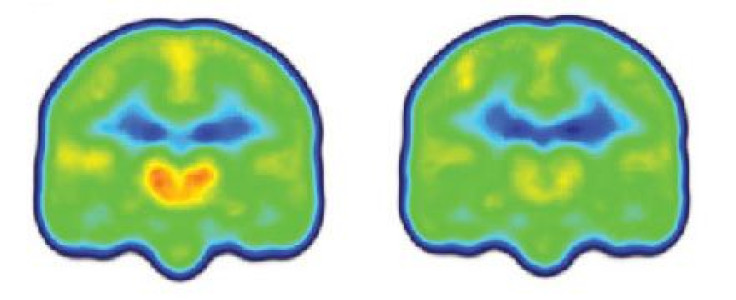
What really interested the investigators was the relationship between TSPO and pain levels. It wasn’t the case that higher pain showed more protein activation. In fact, it was just the opposite.
“While upregulation of TSPO is a marker of glial activation, which is an inflammatory state,” Loggia said, “animal studies have suggested that the protein actually limits the magnitude of glial response after its initiation and promotes the return to a pain-free, pre-injury status.”
This means that people with more pain may actually be expressing less TSPO, sort of as a way to "calm down" the inflammation site, as Loggia explains. "While larger studies would be needed to further support this interpretation, this evidence suggests that drugs called TSPO agonists, which intensify the action of TSPO, may benefit pain patients by helping to limit glial activation."
Up next for the research team is narrowing the focus of glial activation studies. They want to understand how certain forms of pain, like fibromyalgia and rheumatoid arthritis, produce a similar response in the brain. It may be the case, for instance, that each type of pain generates a "glial signature." One day, patients may be able to take different drugs according to the inflammation seen solely in their brain scans.
Source: Loggia M, Chonde D, Akeju O, et al. Evidence for brain glial activation in chronic pain patients. Brain. 2015.



























