Cigna Plans To Cut Opioid Use Among U.S. Customers By 25%
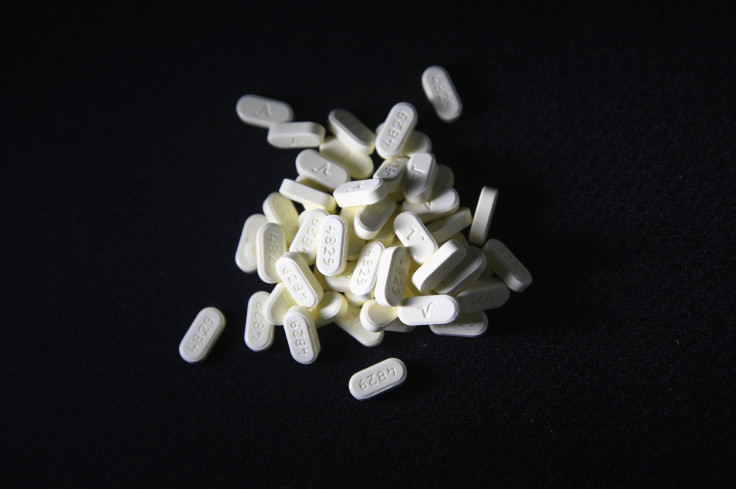
Health insurer Cigna Corp plans to cut its customers' prescriptions for opioid treatments by 25 percent over the next three years, putting its weight behind a U.S. government battle against addictive pain killers.
Cigna, whose plan to be acquired by Anthem Inc would make it part of the nation's largest health insurer, said on Thursday it is backing efforts by state governments to require doctors to check state databases for high-risk customers before prescribing opioid drugs for longer than 21 days.
U.S. President Barack Obama earlier this year asked Congress for $1.1 billion in new funding over two years to expand treatment for a spreading heroin and prescription pain killer epidemic.
Some medical researchers believe an increase in opioid prescriptions over the past few years has caused many patients to become hooked and to seek heroin when their prescriptions expire. In 2014, a record number of Americans died from drug overdoses.
As part of its plan, Cigna is to send doctors information from its own claims databases about its customers' prescription opioid use, enabling doctors to find out if prescriptions have been written elsewhere or if patients have been prescribed drugs to treat opioid addiction.
It will also work with physicians to educate them on prescribing guidelines and access to medication-assisted therapy to treat substance use disorders, Cigna's Chief Medical Officer for Behavioral Health Dr. Douglas Nemecek said in an interview.
Nemecek said Cigna is considering the same types of measures that it has used to moderate use of many medications, including prior authorization, step therapy and the size of the co-pay.
Over 250 million prescriptions are written each year for opioids, Nemecek said. He declined to provide the number attributed to Cigna customers.
(Reporting by Caroline Humer; Editing by Bill Rigby)



























