First-Ever Look Inside A Concussed Brain Reveals Protective Barriers May Be More Porous Than Previously Thought
Although concussions are common, the full effects of this more mild type of traumatic brain injury have been somewhat shrouded in mystery. Until now, using a newly developed mouse trauma model, researchers from the National Institutes of Health (NIH) discovered the brain’s protective coverings may respond to impact more dramatically than previously thought, while brain cells mount an immune response to prevent more widespread damage.
“It was surprising to discover that all these protective barriers the brain has may not be concrete,” Dorian McGavern, Ph.D., National Institute of Neurological Disorders and Stroke (NINDS), stated in a press release. “You can get something to pass through them.” The findings of his research team's new study appear online in Nature.
What is a Concussion?
A concussion occurs when a bump, blow, or jolt to the head changes the way your brain normally works. Concussions can also be caused by a fall or a blow to the body that causes the head and brain to move quickly back and forth. According to a report from the Centers for Disease Control and Prevention (CDC), in 2009 at least 2.4 million people suffered a traumatic brain injury (TBI), and 75 percent of those injuries were mild. Concussions are usually not life-threatening and most people recover quickly and fully, but their effects can be serious. Symptoms can last for days, weeks, or longer and may include headache, fuzzy vision, difficulty concentrating or remembering, difficulty forming thoughts, irritability, and sleeping either more or less than usual. More severe changes, though, spell danger; when any of the following four symptoms occur, it is recommended a person immediately see a doctor:
- Headache that gets worse and does not go away
- Weakness, numbness, or decreased coordination
- Repeated vomiting or nausea
- Slurred speech
Because TBIs, in general, have become a growing concern, a new study of concussions, a form of TBI, provides much needed insight into the damage that may occur following head trauma while also identifying potential therapeutic targets for reducing aftermath damage to the brain.
Brain Trauma
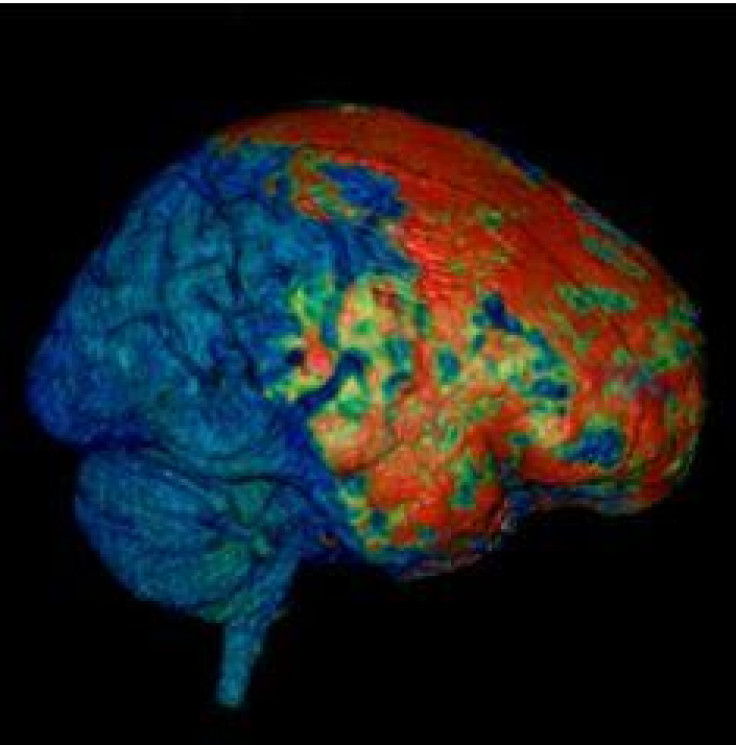
For the study, the research team first examined individuals who had recently suffered a concussion but whose initial scans did not reveal any physical damage to brain tissue. After administering a dye, Lawrence Latour, Ph.D., a scientist from NINDS and the Center for Neuroscience and Regenerative Medicine, and his team watched as it leaked into the meninges, the outer covering of the brain, in 49 percent of 142 patients. They noted that the intact skull bone was porous enough to allow small molecules to get through to the brain and saw how smaller molecules were able to reach the brain faster and to a greater extent than larger ones. After they investigated this human injury, the researchers switched to a newly developed animal model.
“We are using this mouse model to look at meningeal trauma and how that spreads more deeply into the brain over time,” McGavern stated. “In our mice, there was leakage from blood vessels right underneath the skull bone at the site of injury, similar to the type of effect we saw in almost half of our patients who had mild traumatic brain injury.”
The team of scientists observed high levels of reactive oxygen species (ROS) flood the trauma site right after the brain injury happened. Then, the massive accumulation of ROS set up a sequence of events that led to cell death in the brain. The researchers next applied glutathione, an antioxidant that is normally found in our cells, directly on the skull surface after a brain injury. Glutathione works by decreasing levels of ROS molecules and so prevents their effects. In fact, when the researchers applied glutathione immediately after injury, it reduced the amount of cell death by 67 percent and when applied three hours after injury, cell death was reduced by 51 percent.
“This idea that we have a time window within which to work, potentially up to three hours, is exciting and may be clinically important,” McGavern said. Next, the team of researchers filmed what was happening just beneath the skull surface within five minutes of injury and so captured never-before-seen details of how the brain responds to TBI. First, they saw cell death occur in the meninges and at the glial limitans (a slender barrier at the surface of the brain that is the last line of defense against incoming, dangerous molecules). Cell death, they discovered, did not occur in the underlying brain tissue until nine-to-12 hours after injury.
First Responders to Injury
“You have death in the lining first and then this penetrates into the brain tissue later,” McGavern said. Still, almost immediately after head injury, the glial limitans begins to break down and develops holes, providing an entry for potentially harmful molecules to get into the brain. The researchers observed microglia (immune cells that act as first responders in the brain against dangerous substances) quickly ascend to the outer surface of the brain in order to seal the holes.
“If the astrocytes, the cells that make up the glial limitans, are still there, microglia will come up to ‘caulk’ the barrier and plug up gaps between individual astrocytes,” McGavern said. “If an astrocyte dies, that results in a larger space in the glial limitans, so the microglia will change shape, expand into a fat jellyfish-like structure and try to plug up that hole. These reactions … help secure the barrier and prevent toxic substances from getting into the brain.”
Previous studies have suggested that natural immune responses can often lead to severe damage in the brain. By comparison, the current findings show how an inflammatory response to a mild traumatic brain injury is actually beneficial during the first nine-to-12 hours after injury.
Source: Roth TL, Navak D, McGavern DB, et al. Transcranial amelioration of inflammation and cell death after brain injury. Nature. 2013.



























