Gastric Bypass Procedures Not Created Equal, As Researchers Compare Surgery Results
Bariatric surgery — or weight loss surgery — is different for everyone, and the various procedures that can be taken to reduce a person’s obesity have unique consequences.
A new study sought to examine how effective the two most common types of bariatric surgery were — in particular laparoscopic Roux-en-Y gastric bypass (RYGB) and adjustable gastric banding (AGB). The authors concluded that there are risks and benefits involved in both of the procedures, but that RYGB surgery proved to lead to greater weight loss than AGB. At the same time, RYGB had a higher risk of short-term complications and long-term hospitalizations, the authors concluded.
“We found important differences in short- and long-term health outcomes for the AGB and RYGB procedures across 10 health care systems in the United States,” the authors wrote. “Severely obese patients should be well informed of these differences when they make their decisions about treatment.”
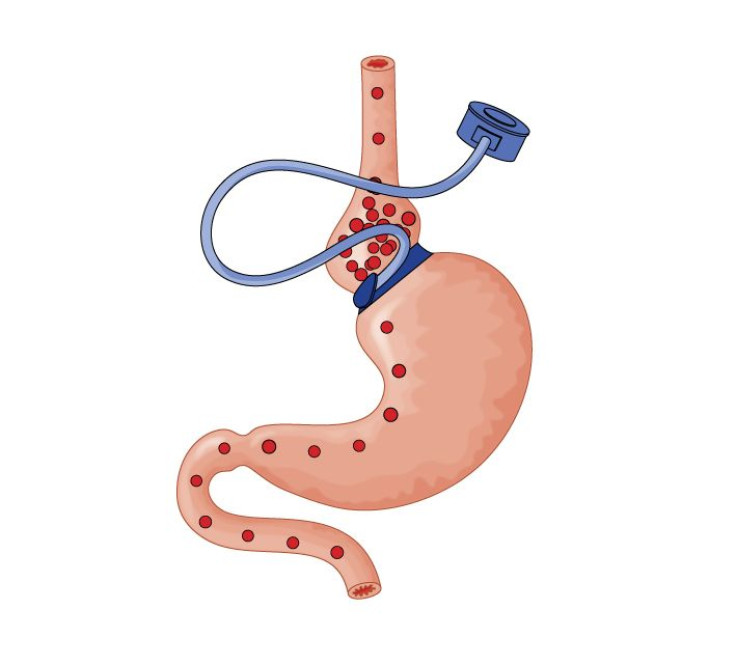
RYGB is the most common weight loss surgery performed in the U.S., and involves separating the upper portion of the stomach from the lower part. The upper portion, known as the pouch, is then connected to a part of the small intestine called the “Rouxlimb,” according to the University of Illinois. The pouch then restricts the amount of food the patient is able to consume, making them feel quite full after only eating a small amount. AGB, or adjustable gastric banding surgery, is sometimes called Lap-Band surgery and involves wrapping a silicone band over the upper part of the stomach. The upper and lower part remain connected through a narrow part through the band, but the band ultimately restricts the amount of food the patient can eat. The food moves through the narrow part so slowly that the patient will feel full for longer.
In the study, the researchers examined 7,457 patients who had undergone some form of bariatric surgery from 2005-2009, then followed up with them in 2010. They studied changes in body mass index (BMI) as well as any major adverse outcomes, such as death, venous thromboembolism, and failure to be discharged from the hospital. Results showed that the average maximum BMI loss was 8.0 for AGB patients, and 14.8 for RYGB. Meanwhile, a higher amount of RYGB patients experienced major adverse events after the surgery than AGB patients.
“The study… adds another important perspective to our understanding of the outcomes of bariatric surgery procedures,” Dr. Justin Dimick and Dr. Jonathan Finks of the University of Michigan, who were not involved in the study, wrote. “This study confirms what we know about the perioperative safety: that bypass is higher risk than laparoscopic band placement... [t]he results… also confirm what we know about weight loss, namely, that gastric bypass is about twice as effective in the intermediate term (2-4 years) as the adjustable gastric band.”
“Perhaps the most important contribution of this study lies in the methods and data sources for two important reasons,” they continued. “First, the data used in this study give us a picture of what is happening in the real world — a range of hospitals and practice settings — by linking hospital-billing data to electronic health care records. …Second, this study demonstrates the feasibility of using these large, readily available data sets for meaningful comparative effectiveness research.” Ultimately, patients looking into bariatric surgery should be aware of the pros and cons of both procedures.



























