HIV Treatment May Someday Include Monoclonal Antibodies: Lab-Created Molecules Could Prove To Be Profoundly Effective
New published online today in Nature provides evidence that monoclonal antibodies — 'designer molecules' produced in a lab to target specific disease — may be an effective therapy for the treatment of human immunodeficiency virus (HIV).
"Our data demonstrate, for the first time, profound therapeutic efficacy of broad and potent HIV-specific monoclonal antibodies in rhesus monkeys chronically infected with a highly pathogenic simian-human immunodeficiency virus," the study's lead author, Dan H. Barouch, M.D., Ph.D., director of the Vaccine Program at the Ragon Institute of MGH, MIT, and Harvard, stated in a press release.
Simian-human immunodeficiency virus is a version of HIV that occurs in monkeys.
What are monoclonal antibodies?
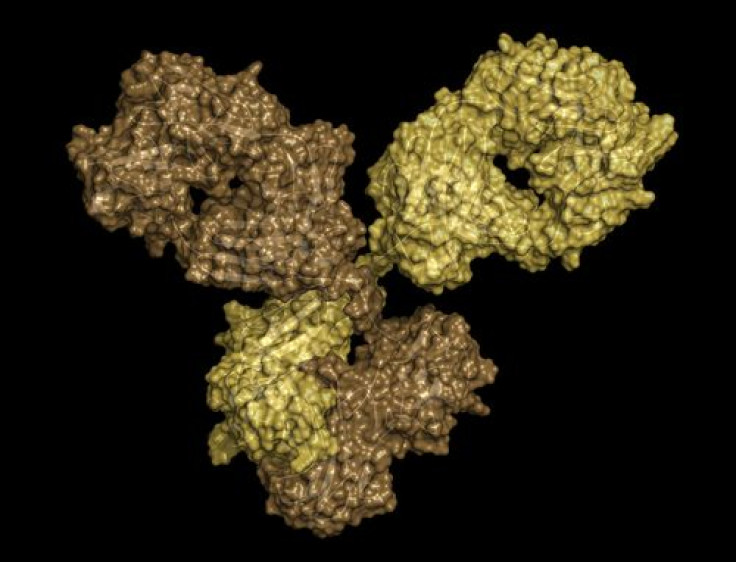
To understand how monoclonal antibodies work, it is necessary to understand the mechanisms of the immune system. The body’s immune system attacks and destroys foreign substances. Specifically, the body responds to the introduction of foreign proteins, called antigens, by producing antibodies. An antibody is actually a protein that functions as a ‘marker’ specific to the antigen. It circulates in the body until it finds and attaches itself to the antigen, and after binding to it, the molecule can be recognized and destroyed by phagocytes, which destroy the cells containing the antigen.
In a laboratory, a scientist can make many copies of a specific antibody, called monoclonal antibodies (mAbs). ‘Monoclonal’ cells are produced by repeated replication of a single antecedent cell. During the past 20 years, mAbs have been designed to target a certain antigen, such as one found on cancer cells, and so have been useful in treating disease.
The standard treatment for patients with HIV, though, is antiretroviral therapy. These therapies, though, have drawbacks: they are unable to cure HIV infection and, though effective for most patients, are limited because of resistance and toxicity issues. In the past few years, researchers have begun to consider antibodies as a potential new treatment for HIV because they would work through a mechanism distinct from that of antiretroviral treatments.
"Antibodies directly target free virus as well as virally infected cells, whereas existing antiretroviral drugs only inhibit the replicating virus," explains Barouch. "Antibodies may, therefore, offer a unique therapeutic strategy that could potentially be combined with antiretroviral drugs."
In a preclinical study — one that does not involve humans — Barouch and his team administered a cocktail of HIV-specific mAbs or single mAbs into rhesus monkeys chronically infected with simian-human immunodeficiency virus.
"The antibody treatments resulted in a rapid and precipitous decline of virus in both blood and tissues of the infected monkeys," notes Barouch. Following a single antibody infusion, viral loads dropped sharply to undetectable levels within three to seven days. The team of researchers also found cell-associated virus levels to be reduced in the blood, lymph nodes, and the gut.
Most impressive, antibody infusions boosted the monkeys' own immune responses against the virus, which appeared to have long-term benefit. The researchers noted that in most cases, the virus rebounded when antibody titers declined after a certain time period (56 days median), but some cases proved exceptional. “Remarkably, the subset of animals with the lowest starting levels of virus maintained undetectable viral loads for the duration of the study, in the absence of further antibody infusions," Barouch stated in a press release.
The researchers believe their data might inspire the development of new monoclonal antibodies-based therapies for HIV in humans.
"Monoclonal antibodies in conjunction with antiretroviral drugs can be explored for treatment intensification, pre- and post-exposure prophylaxis, and virus eradication strategies for HIV in humans," Barouch stated in a press release.
Source: Barouch DH, Burton D, Nussenzweig M, et al. Monoclonal antibodies show promise as effective HIV therapy. Nature. 2013.



























