HPV Improves Survival Rates for African-Americans With Throat Cancer
Human papillomavirus (HPV) is known to increase one’s risk of being diagnosed with cervical cancer, but a new study provides research that suggests HPV may improve survival among African-Americans suffering with throat cancer.
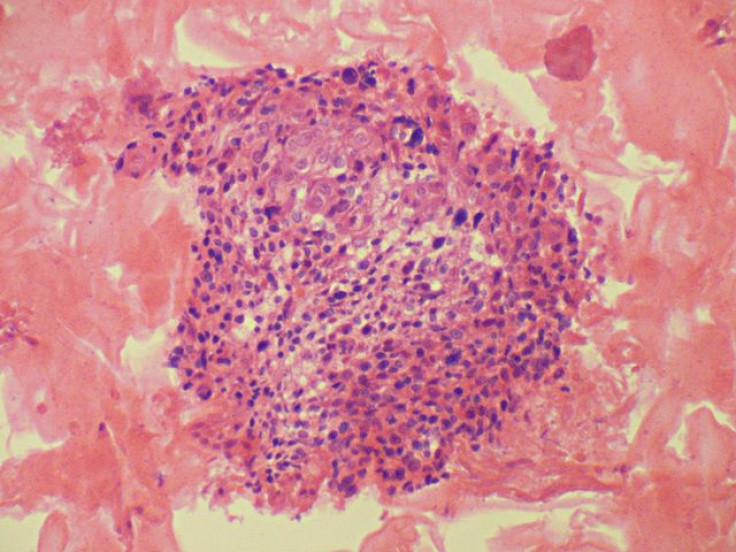
Throat cancer, and more specifically oropharyngeal cancer, affects parts of the throat, base of the tongue, tonsils, the palate and wall of the pharynx.
The study, which was conducted by the Henry Ford Medical Group, consisted of 51 participants who were HPV positive, of those 42 were African-Americans, and 67 participants were HPV negative.
Researchers discovered that general survival rates for HPV negative African-Americans with oropharyngeal cancer are lower than African-Americans who have been diagnosed with HPV. The results also stated, not only do HPV-negative African-American have a lower survival rate compared to African-Americans with HPV, but they also have a lower survival rate in comparison to Caucasians, both HPV positive or negative.
The study also displayed African-Americans are less likely to be diagnosed positive with HPV. People 50 or older are also less likely to be HPV positive. Individuals with late stage oropharyngeal cancer are likely to be single and HPV positive. HPV negative patients are at 2.9 times the risk of death compared to HPV positive patients.
According to lead author Maria J. Worsham, Ph.D., and director of research in the Department of Otolaryngology-Head & Neck Surgery at Henry Ford, the report also provides a substantial amount of evidence that suggests HPV is a racially-linked sexual behavior lifestyle factor that has a significant effect on the survival rates of African-American and Caucasians.
The American Cancer Society believes about 35,000 people nationwide will get oral or oropharyngeal cancer in 2012. Of those diagnosed with oropharyngeal cancer, 6,800 will lose their battle. Oropharyngeal cancer is more common in men than women.
Study results will be presented Sunday, July 22 at the 8th International Conference on Head and Neck Cancer in Toronto. The research was funded by a National Institutes of Health grant.



























