Lab-Grown Cancers May Lead the Way to Custom Treatments
It's been a two-decade nightmare: a 24-year-old has endured over 350 surgeries on recurring tumors that have appeared in his throat and in his lungs. The young man, who asked not to be named, said that the growths first started to appear when he was three or four years old. The tumors would cause shortness of breath and hoarseness in his voice, and he needed to have surgery every seven to 10 days. When he entered his twenties, doctors said that the growths became life-threatening, crushing his airway.
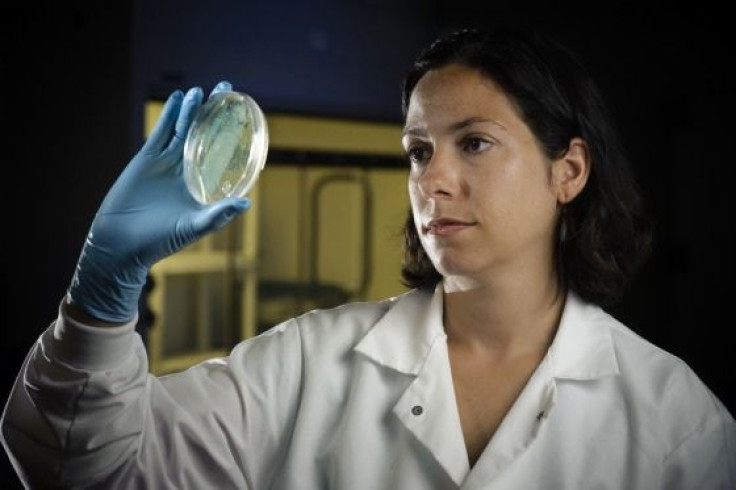
So two years ago, doctors at Georgetown University Medical Center, in Washington, DC, tried using a new procedure, which could help with custom treatment of the millions of people who suffer from similar illnesses every year. The procedure is an answer to a unique question: how can we keep cancerous cells alive forever once they leave the body? Doctors seem to have found an answer. They take a few cells from a biopsy and grow them in a petri dish. After two weeks, scientists test numerous drugs or combinations to discover the best course of action.
In the case of the 24 year old, an information technology specialist, the cells turned up an answer: a drug used to treat a certain type of blood cancer and some other conditions could help.
But the answer was surprising because the young man does not technically have cancer, so his doctors would have never come up with that line of treatment. As explained in the case study published in today's issue of the New England Journal of Medicine, he has recurrent respiratory papillomatosis, or RRP. The disease is caused by infection at birth with HPV, a virus that can cause genital warts and cervical cancer in women. RRP causes wart-like growths in the throat, which are normally not fatal but can prove extremely dangerous if they spread to the lungs.
While it has become routine for researchers to grow diseases in lab dishes, cancer cells seemed to be impossible because they do not easily grow in cultures. But the treatment could prove to be heaven-sent for cancer patients, by showing whether a treatment will work without side effects or wasted time. In this case, the first drug proved ineffective, while a second worked but at a dose so high that it would be lethal. The third drug did the trick.
The next step is to see whether the approach would work on other cancer patients, but the IT specialist is pleased with the outcome so far. While he still has to make appearances in surgical facilities, his visits are down from every week to every three months.
So far Dr. Richard Schlegel and his lab at Georgetown have grown prostate, breast, lung, and colon cancer cells. Researchers at Georgetown are currently seeking a patent on the process.



























