Living Life With MS: The Symptoms And Sacrifices As Told By Patients, Caregiver

If you were to meet Kristin Decker, you would never know she’s been living with multiple sclerosis (MS) for nearly five years. At 28 years old, Decker awoke one morning with droopiness on the left side of her face, numbness, and the loss of her vision. What she described were the first symptoms of MS, a disease that turned Decker’s immune system against her and continues to attack the protective layer over her nerves, known as myelin.
When myelin is damaged it disrupts the communication between the brain and the rest of the body, ultimately deteriorating the nerves themselves in an irreversible process, according to the Mayo Clinic. Currently, there is no cure for the 2.5 million people in the world like Decker. Each person’s condition varies with their own symptoms, from mild forms of relapsing-remitting, to the more severe and unrelenting secondary and primary-progressive stages.
“It really happened so quickly,” Decker told Medical Daily. “It was really in a matter of a week that I lost vision, my face was dropping, and I had numbness. Within two weeks, I had symptoms, I was in the hospital, and I was diagnosed and sent on my way.”
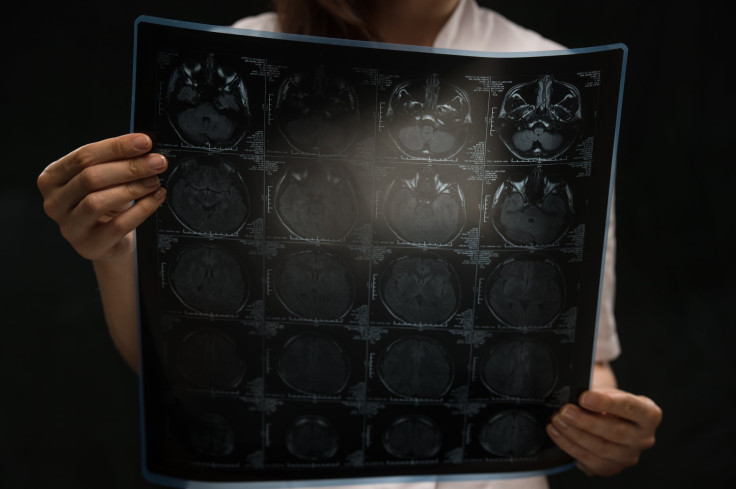
Decker called urgent care and they told her to go to the emergency department. She eventually saw a neurologist who, after testing, wrote her a prescription for an MRI and told her they were pretty sure she had MS. After they placed her on steroids, administered a spinal MRI, and a spinal tap, Decker was officially diagnosed with MS. Decker immediately met her diagnosis feeling frightened. The only person she ever knew who had MS was her aunt’s sister, who had a more severe and progressive form of MS. Decker began to think her future would be lived out in a wheelchair.
Life had drastically changed in a short amount of time. Everything became trial and error. She started taking daily injections of Copaxone when she was first diagnosed and then was relieved to switch over a twice-a-day pill of Tecfidera. She calls herself lucky for having a quick diagnosis and a mild enough form that allows her to be involved in raising donations and awareness.
Decker, with the encouragement of her friends and family, decided to get involved in the search for a cure by forming a team to raise crucial funds and walk in Jersey City’s National Multiple Sclerosis Society’s Walk MS. In the last four years, Decker and her team “All Hands on Deck” have become top fundraisers, collecting over $60,000 for the National Multiple Sclerosis Society. She describes it as her Christmas. The night before the big day she says she could hardly sleep, and when the day finally presented itself, she was humbled by the generosity and support from family, friends, and coworkers.
“I’ve learned that health, especially diet, plays so much into how you feel,” she said. “The paleo diet eliminates dairy and grain, which causes inflammation, and because you already have inflammation with MS, anything that you can eliminate makes such a difference. When I have cheat days, afterwards I’m like ‘that was such a bad idea. I’ve been very lucky with my diagnosis because I have a milder case. But heat, stress, and lack of sleep are points when I’m like, ‘OK, I need to step back and take it easy.’”
Over time, living with MS has become easier for Decker to adapt to and accept. Since her diagnosis, she’s entered into an entirely new community through social media, her local gym in Hoboken, and online support groups. She’s also joined the National MS Society’s Community Engagement Committee in order to become more involved in community-led events. Through community-based connections, Decker believes people have greater access to information, which allows them to modify their diagnosis and curb their symptoms. No two people have the same MS, but she’s found connecting with people and learning about their experiences helps impact her own condition. Diet and exercise have been an outlet and, in a way, a form of treatment for her.
Inspiration to Overcome Obstacles
Before February 2010, exercise had been a large part of the then-26-year-old Daniel Buckelew’s life. He was an athlete all throughout college and was in graduate school working on his Master’s in Business Administration while working as a financial analyst full time when the symptoms began to manifest. So, he took his primary care doctor’s advice to go to a neurologist, and after getting an MRI, the scan revealed lesions, which served as grounds for his diagnosis.
“My initial reaction was confusion,” Buckelew told Medical Daily. “I look at the MRI and see these white spots all over them and say, ‘What does that mean?’ My father reached out to somebody who he knew had MS and they immediately told him I should be going to a specialist, thankfully. It was over the course of six to eight months where I was with a general neurologist not getting the support that I really needed.”
Not receiving specialized care started Buckelew on a slow road to recovery. Walking and balancing were a struggle, he says, and despite his stubbornness he began to use a cane because his episodes were so uncertain he couldn’t leave his house without it. Slurred speech, cognitive issues, and bladder and spasm problems soon became a regular part of his life.
“You should’ve seen me at my first few visits to his office,” Buckelew said. “I would bring a family member, whether it was my wife, my mother, my father, and then just have them there as a scribe to take notes, just because at the time I was having quite a bit of cognitive issues and was not able to recall everything. Just to have those notes in order to look back and see where the conversation was and what we had discussed.”
This year, Buckelew has been named the “Most Inspirational Walker” at the National Multiple Sclerosis Society’s Walk MS in Roxbury, N.J. Early on in his diagnosis, it was never something he could have imagined for himself, he says. There were 30 people registered on his team alone, not including the friends and family each registrant brought along for their fifth annual walk around Horseshoe Lake. It was humbling and exciting to be recognized, he says, and to look back and remember where he was and where he is now today is unbelievable. It took him three years of gradual progress before he was able to run a 5K again, and eventually two 10-mile Tough Mudder races.
It’ll be his last year walking at Walk MS in Roxbury. Before Buckelew’s diagnosis, he began working at Sanofi, a global healthcare research and drug developer that soon after acquired Genzyme, a company that specializes in specialized therapies for patients. As of March 23, 2015, Buckelew took a position at Genzyme’s MS franchise in Cambridge, Mass., where he, his wife, and their 2-year-old daughter will be relocated and join their local MS Walk chapter.
“For me, I really look to do whatever I can in the fight against MS and bring awareness to it,” Buckelew said. “I saw this opportunity of working with the Genzyme MS position as one of the best ways to get involved. It’s something I’ve been wanting to do for a while because it’s something I hold very close. I couldn’t be more excited about the opportunity that I’ve been given.”
15 Years of Dedicated Care
For BAYADA Home Health Care aide Kelly Maltes, MS has been a part of her life from a caretaker’s standpoint. Maltes has been taking care of the same client for eight hours, seven days a week, for 15 years. Symptoms began arising in the client’s teenage years in the form of blurry vision. After seeing an ophthalmologist, they suspected it was MS, but an official diagnosis wasn’t made until two years into her new marriage.
MS symptoms can begin anywhere between 10 to 80 years of age, according to the Cleveland Clinic. Now at the age of 52, she’s lived most of her life with the disease, of which Maltes has been an intrinsic part. Maltes watched her client undergo experimental chemotherapy treatments at Columbia Presbyterian and for a time showed significant promise. Her condition even plateaued and then went into remission. But in the last two years, her condition has taken a turn for the worst, as Maltes explained.
“Since it’s progressing more and more, it’s difficult to walk,” Maltes told Medical Daily. “She’s basically housebound. She’s really not walking much anymore. She can’t do whatever she was used to do. After the chemo treatment, she was great. I was able to take her everywhere, and I used to wheel that wheelchair everywhere.”

In the beginning, they would go to support groups together and the National MS Society Walk MS in Bayonne where her client was one of the top fundraisers. It was there Maltes learned how different everyone’s symptoms were and how their dispositions varied from acceptance to happiness. Throughout the years, as Maltes’s client’s condition worsened, she realized the depression and anxiety was starting to take over and a newer, more difficult stage of the MS presented itself.
“The problem is she has depression and anxiety,” Maltes said. “It’s very common for people who have MS. They could be pleasant, but they could be moody and it’s something that you have to keep in mind and approach with patience. She’s had MS for so many years, but she cannot accept she can’t do what she used to do. She thinks, or wants to think, she can do everything on her own. When she realizes she can’t, she gets frustrated.”
At one point, her client started to experience twitching and stabbing pain in her mouth. She went to the hospital, where they determined it was dental problems and proceeded to remove every tooth and nerve from her mouth. Yet, the pain persisted. Maltes took to the Internet, because, she says, it used to bother her seeing her client suffer that way. It was then she found one of the rare symptoms of multiple sclerosis was trigeminal neuralgia. The trigeminal nerve is one of 12 pains of nerves attached to the brain, making it a neuropathic pain, according to the National MS Society.
Her client was brought to her neurologist specialist, who confirmed Maltes was correct. They placed her on a regiment of pills, and although some of them worked, many did not agree with her. The trigeminal neuralgia was kept under control, but her condition continued to rapidly decline. Maltes says it won’t be long before she’s bedbound, a 15-year decline she’s become intimately familiar with every step of the way.
“It’s difficult for the caregivers,” Maltes said. “It’s not easy. You have to have a lot of patience and be very understanding. Of course, it affects me on a personal level, because I want to do the best I can. I do as much as I can for her, but as much as I do, seeing her not getting better, of course makes me sad. It makes me anxious, too, because I want to help. I keep reading articles to help me do the best I can for her. You have to be strong when caring for a person with MS.”



























