Lou Gehrig’s Disease Treatment On The Horizon? Engineered Stem Cells Could Be The Key
Amyotrophic lateral sclerosis (ALS), more commonly known as Lou Gehrig's disease, is a neurodegenerative disease in which patients slowly lose their ability to talk, breathe, and even swallow. There have been few treatments that only moderately slow the progression of the disease and much of the focus has been on management of symptoms and care of patients. Much research is being performed to determine how the disease progresses, what causes it, and how it can be fixed.
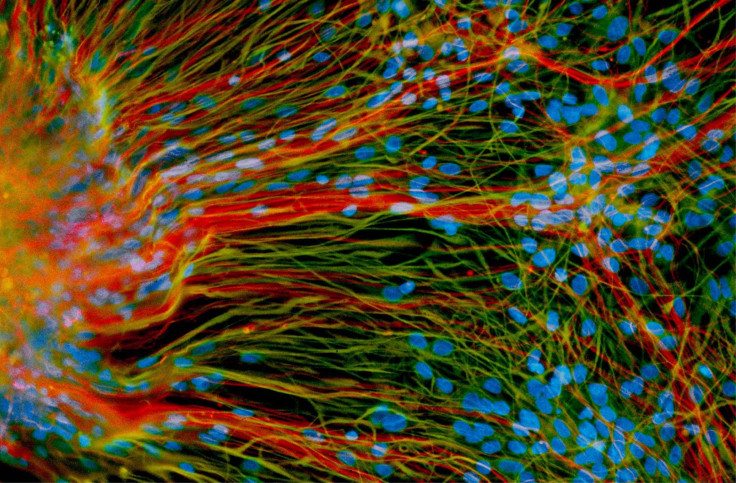
New research out of the University of Wisconsin School of Veterinary Medicine, published in the Nature journal Molecular Therapy, holds some promise for future treatments for people afflicted with the disease. Scientists took adult human stem cells, purified from bone marrow, and modified them to produce growth factors that encourage the regrowth of new nerve cells. These engineered stem cells were then implanted directly into the muscle of rats, which had been genetically engineered to have symptoms of ALS and are commonly used in ALS research.
The stem cells were engineered to produce vascular endothelial growth factor (VEGF), a protein that encourages the growth of new blood vessels, which supply oxygen and nutrients to parts of the body. The study found that just delivering the blood vessel growth factor increased survival of the ALS-afflicted rats and delayed the onset of the disease. The lead researcher on the project, Dr. Masatoshi Suzuki, had previously shown that using another growth factor, glial cell line-derived neurotropic factor (GDNF), near the junction between nerves helped them to live longer. By combining both VEGF and GDNF, Dr. Suzuki said that the real advance was using stem cells that produced both growth factors. "In terms of disease-free time, overall survival, and sustaining muscle function, we found that delivering the combination was more powerful than either growth factor alone. The results would provide a new hope for people with this terrible disease," said Dr. Suzuki.
The thought with ALS progression is that much of the damage to neurons in the periphery occurs close to the spinal cord, which brings signals from the brain to the rest of the body. But Dr. Suzuki has found that the end of the nerve that activates the muscle is typically first affected by the disease. The stem cells used in this experiment did not turn into neurons, but rather were used as factories to produce growth factors that would encourage nerve cell survival. The modified stem cells survived in the rats for up to nine weeks, long enough to result in a positive impact on disease progression. The technique relied on keeping existing nerve cells healthier and alive, rather than other approaches that use stem cells to create new neurons to replaced damaged ones.
"These motor nerve cells have extremely long connections, and replacing these cells is still challenging. But we aim to keep the neurons alive and healthy using the same growth factors that the body creates, and that's what we have shown here," said Dr. Suzuki.
By using adult stem cells, the research group avoided a problem first encountered when trying to perform stem cell treatments. When embryonic stem cells were used in transplant treatments, they had a propensity to turn into tumors, as they grow at a fast rate and are moved into a new environment with different signals than they are used to. By using adult cells, the risk of this was eliminated and became more clinically relevant, as an adult's own bone marrow stem cells could be used to treat the disease.
Source: Krakora D, Mulcrone P, Meyer M, et al. Synergistic Effects of GDNF and VEGF on Lifespan and Disease Progression in a Familial ALS Rat Model. Molecular Therapy. 2013.



























