Lung Cancer Screening For Heavy Smokers Recommended By U.S. Preventative Services Task Force
The U.S. Preventative Services Task Force, a panel of experts appointed with setting guidelines for screening and preventing major illnesses, has issued new guidelines for lung cancer screening in high-risk populations, particulary older people with a long history of smoking. Policy makers and researchers predict that the new policy could save as many as 20,000 lives each year.
Who Should Get Screened For Lung Cancer?
While it is still in draft form open to public comment, the tentative guideline currently recommends that people ages 55-79 who have a 30 pack year history of smoking get screened annually, even if they have quit as long as 15 years ago. Pack years are calculated by multiplying the number of years as a smoker by the number of packs per day smoked. For example, a person who smoked 1 pack a day for 30 years and a person who had smoked 2 packs a day for 15 years, both have a 30 pack year history. An estimated 10 million people in the U.S. fit this criteria.
People who fit these criteria should be screened by low-dose computed tomography, or CT scan. This imaging technology consists of an X-ray machine that makes a series of detailed pictures, and could detect much smaller tumors earlier in development than the current standard — chest X-rays.
The recommendations are unprecedented. Until recently, there was little evidence to support screening for lung cancer using any type of imaging, and thus no screening guidelines. By the time tumors were large enough to be detected on the standard chest X-ray, it was often too late to treat with surgery.
The results from a large-scale clinical trial from 2010 changed that. Researchers from the National Cancer Institute followed 53,000 patients and found that mortality from lung cancer could be reduced by 16 percent if patients at the highest risk were screened.
For patients at lower risk for lung cancer, the risk for complications resulting from testing outweighs the potential benefits. A CT scan could raise suspicions of lung cancer where there is none, leading to invasive biopsies and maybe even unnecessary surgeries.
Lung Cancer Is The Leading Cause Of Cancer Death
Given the severity of lung cancer as a public health problem, the new guidelines could make a huge impact. Lung cancer is the leading cause of cancer death in the U.S., killing 160,000 people a year. Nearly 90 percent of patients diagnosed with lung cancer die from it, as it is usually discovered too late.
The most common type of lung cancer, non-small cell lung cancer, could be cured if its caught early.
The U.S. Preventative Services Task Force recommendations are important because they often set the standard for what services are covered by insurance. Under the Affordable Care Act, preventive health screenings, including these annual CT scans for high-risk patients, would be offered to qualifying beneficiaries with no co-pay.
These recommendations could transform how lung cancer is viewed by the public. Often perceived as tantamount to early death, lung cancer now has a hopeful intervention. But that shouldn't detract from efforts to prevent lung cancer from occuring.
"The main message is unchanged," Dr. Harold E. Varmus, the director of the National Cancer Institute, said. Don't smoke.
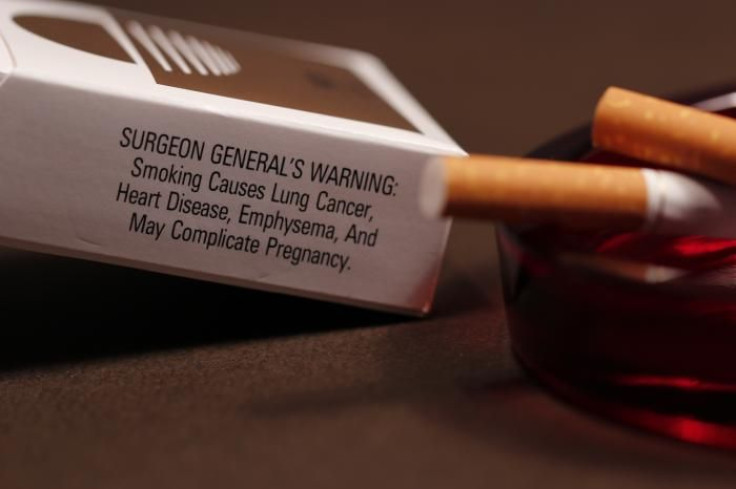
Smoking is the culprit in about 85 percent of all lung cancer deaths.
To determine whether you should be screened annually for lung cancer, use Memorial Sloan Kettering's lung cancer screening decision tool online.



























