Marijuana Linked To Poor Memory In Teens: Pot May Cause Abnormal Brain Function And Schizophrenia-Like Symptoms
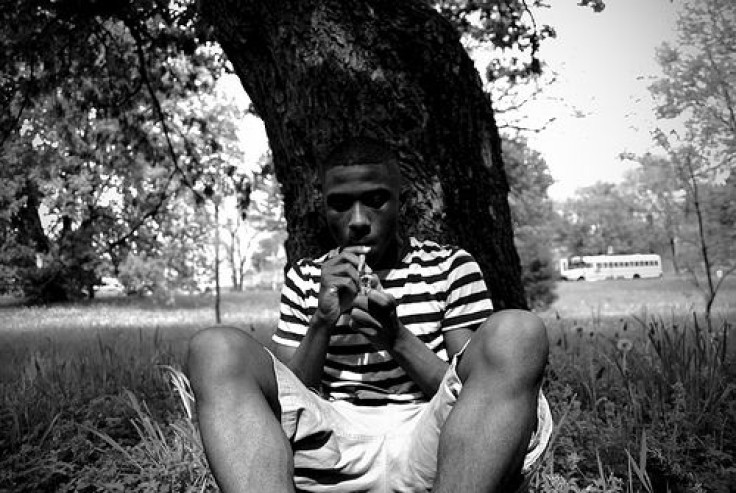
Despite the numerous advances made in the field of medical marijuana research, a new study from Northwestern University Feinberg School of Medicine (FSM) shows that the drug still displayed negative cognitive effects among teenagers who smoked daily for a period of three years.
The effects included a poorer working memory, characterized by an inability to quickly process information and, if needed, turn short-term memories into long-term memories. The study also showed it led to an increasingly abnormal brain structure and symptoms similar to those found in schizophrenia patients. When researchers followed up on the 16- and 17-year-olds in their early twenties, the subjects had been drug-free for two years; however, that’s when the scientists observed abnormalities and memory loss, signs that even short-term chronic use may leave lasting, long-term effects.
Lead author of the study, Dr. Matthew Smith, said the study has particular salience because of the ongoing national debate about decriminalizing, and indeed, legalizing, marijuana. So far, only Washington and Colorado have fully legalized the substance. Meanwhile, 19 states have legalized it for medicinal purposes.
"The study links the chronic use of marijuana to these concerning brain abnormalities that appear to last for at least a few years after people stop using it," Smith, an assistant research professor in psychiatry and behavioral sciences at FSM, said in a statement. "With the movement to decriminalize marijuana, we need more research to understand its effect on the brain."
Teens that began using marijuana earlier were found to display greater brain abnormalities than teens that started consuming the drug later in life. This signaled to researchers a greater susceptibility in the younger teens’ growing brains. Many of the processes normally implicated in frequent marijuana use were found damaged or their growth otherwise stunted, including collapsed memory-related structures — pointing to a shrinkage of neurons — and deficient processing in the pre-frontal cortex, which controls motivation and was found in a similar state among the team’s schizophrenic subjects. Such a link concerned the researchers, as it suggests drug use may predict or enhance certain mental disorders.
"The abuse of popular street drugs, such as marijuana, may have dangerous implications for young people who are developing or have developed mental disorders," said co-senior study author Dr. John Csernansky, chair of psychiatry and behavioral sciences at FSM and Northwestern Memorial Hospital. "This paper is among the first to reveal that the use of marijuana may contribute to the changes in brain structure that have been associated with having schizophrenia."
While the study’s effects seem to point toward closely monitored drug use, if any, Smith and his colleagues conceded that they only examined participants’ brain health at one point in time. A longitudinal study is needed to fully assess the drug’s long-term effects and to isolate the drug as the sole mediator of those effects. Meanwhile, 90 percent of the 15 schizophrenic subjects began heavy marijuana use before developing the disorder, pointing researchers in a hopeful direction.
Subjects with heavy drug use and those with heavy drug use and schizophrenia both showed abnormal changes in their brains. But subjects with the mental disorder showed greater deterioration in the thalamus region of the brain, which, among other things, controls learning and memory, and liaises between surrounding regions of the brain.
"A tremendous amount of addiction research has focused on brain regions traditionally connected with reward/aversion function, and thus motivation," noted co-senior study author Dr. Hans Breiter, professor of psychiatry and behavioral sciences. "This study very nicely extends the set of regions of concern to include those involved with working memory and higher level cognitive functions necessary for how well you organize your life and can work in society."
Given that people with a history of schizophrenia in the family increase their risk for developing the disorder with the consumption of marijuana, Smith and his colleagues urge people — parents, especially — to consider the risks of teen marijuana use, not only in the short-term, but as their brains continue to grow and eventually solidify in their mid-twenties.
"If you have schizophrenia and you frequently smoke marijuana, you may be at an increased risk for poor working memory,” cautioned Smith, “which predicts your everyday functioning.”
Source: Smith M, Cobia D, Wang L. Cannabis-Related Working Memory Deficits and Associated Subcortical Morphological Differences in Healthy Individuals and Schizophrenia Subjects. Schizophrenia Bulletin. 2013.



























