MERS Virus Spread Through Saudi Arabian Hospitals; May Be Deadlier Than SARS Outbreak
An international team of specialists, who went to Saudi Arabia to analyze the new Middle East respiratory syndrome (MERS) outbreak, reported Wednesday that the virus appeared to spread easily between people in a hospital setting and is potentially more deadly than the SARS outbreak 10 years ago.
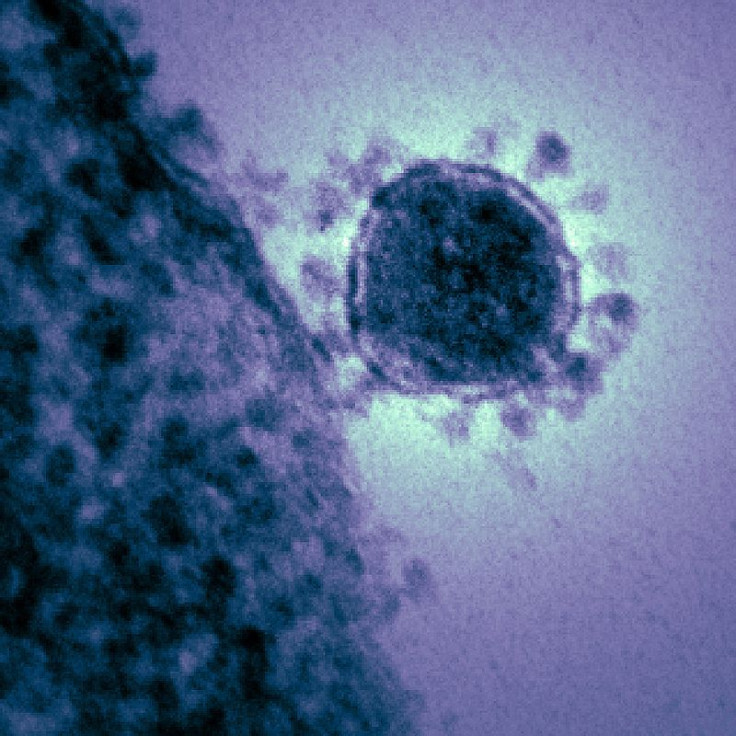
MERS, a viral respiratory disease caused by the coronavirus MERS-CoV, was found to be easily transferable — at least in the Saudi Arabia hospital setting where it rapidly spread. According to the long awaited report published in the New England Journal of Medicine (NEJM), at one point, the virus spread five generations through person-to-person infection.
"To me, this felt a lot like SARS did," said team member, Dr. Trish Perl, a senior hospital epidemiologist at Johns Hopkins Medicine.
MERS-CoV is a cousin of severe acute respiratory syndrome (SARS); however, it is not the same coronavirus. According to the World Health Organization (WHO), coronaviruses are a large family of viruses that could have a range of illnesses from the common cold to SARS. In September 2012, WHO reported the first cases of pneumonia that was caused by MERS-CoV, and has since reported 64 cases. Thirty-eight of those cases led to death, and 32 of the deaths occured in Saudi Arabia.
The ease at which the virus has to this point moved through people and health care facilities is what has set leading health care authorities to demand more testing and better record keeping of the outbreaks. The chains of transmission may have stretched beyond five generations, and without knowing the origin of this new virus, the threat is that much greater. Doctors around the world share a building frustration with their inability to successfully treat their patients.
"We need more information from other countries to find out what the best treatment is," said Dr. Clemens Wendtner, a professor of Medicine and Assistant Medical Director at the University of Cologne in Germany, who treated a MERS patient who later died in Munich. "Our patient got everything possible and it still didn't help him."
After mapping out MERS-CoV cases within health care facilities, investigators found that face-to-face contact or time spent in the same area as an infected patient leads to a much greater risk than infected patients sharing the same caregivers or equipment, NEJM reported. The findings looked at the relationship between infected family members, patients, and hospital staff in order to see how easily the virus is transferred and through what modes it's most quickly infecting individuals.
At the time of the investigation, 23 people in Saudi Arabia were infected, 11 of which died. Eight of the infected patients were transferred between facilities or hospitals — a factor that researchers said increased the likelihood of infection transfer.
According to the study, "The rapid transmission and high attack rate in the dialysis unit raises substantial concerns about the risk of health care-associated transmission of this virus."
The origins of the disease are unknown, which makes it a greater threat to the health care staff within infected facilities. Perl said how the disease is spread isn't exactly known either. Each case could have infected others differently, whether it's from sneezing or coughing droplets, or if it moves through a more indirect route. Some hospital patients that weren't within the vicinity of an infected person also somehow contracted the virus, which baffles doctors all the more.
"In the right circumstances, the spread could be explosive," warned Perl.
Scientists, researchers, and leading authorities on disease control, such as the Centers for Disease Control and Prevention (CDC), are comparing MERS to the defining characteristics of SARS, a disease that spread in 2002 and wasn't fully contained until 2004. According to Mayo Clinic, SARS was a contagious and fatal disease, much like MERS. SARS death toll rose to about 770 after infecting over 8,000 individuals in nearly 25 different countries.
It is still unknown if MERS also infects through super-spreaders, people who can carry and transmit the disease without demonstrating any symptoms, a threatening feature of SARS. To this point the numbers are scary: there has been a 65 percent fatality rate in the Saudi Arabia outbreak. For comparison, over the entire SARS outbreak, the death rate was only eight percent. On the other hand, SARS infected significantly more people, and there are few who would say at this point that MERS is deadlier than SARS. But the threat is still there.
"We understand too little about this virus when viewed against the magnitude of its potential threat," said General Dr. Margaret Chan, director of WHO.
Source: Assiri A, McGeer A, Perl TM, Price CS. Hospital Outbreak of Middle East Respiratory Syndrome Coronavirus. The New England Journal of Medicine. 2013.



























