More Than Half Of Women With Dense Breasts Don't Need Additional Cancer Screening, Despite Current Recommendations
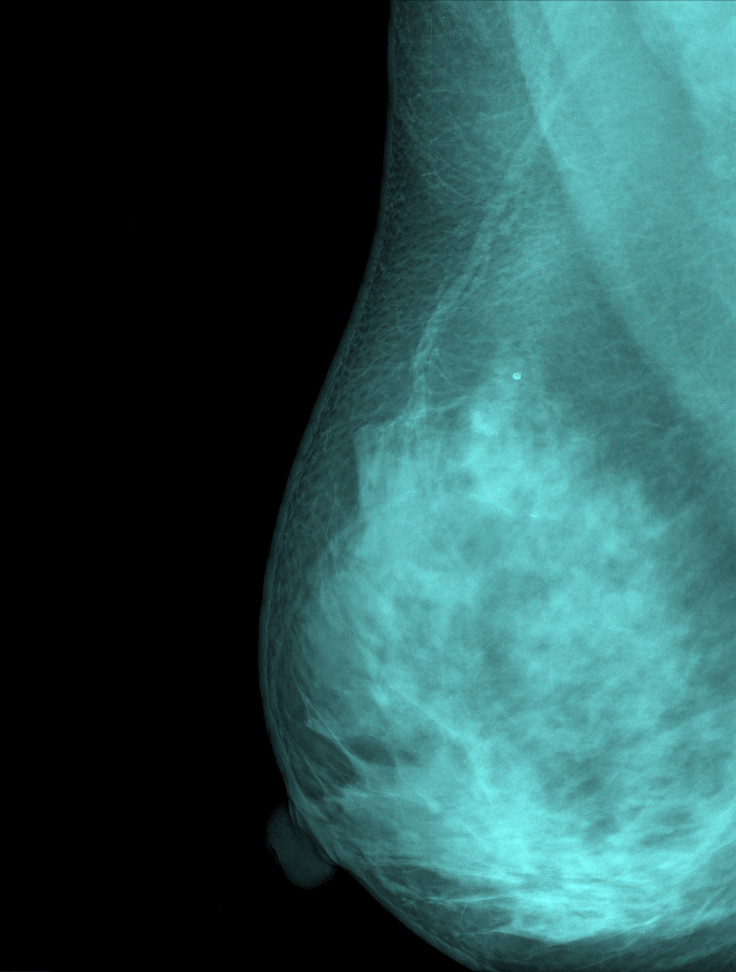
Fun as they might sound to a growing teenage boy, dense breasts are more trouble than they’re worth. That’s because many oncologists say that not only can dense breast tissue mask potential tumors on a mammogram, but that it itself can be a risk factor for eventual breast cancer.
That’s why nearly half the country, or 21 states, has passed legislation advising doctors to alert their patients should they have dense breasts and to recommend that they undergo additional cancer screening methods like a MRI scan. On its face, these recommendations seem like a common sense step for older women to take, but, according to a new study from the Annals of Internal Medicine, it may actually be an unneeded one for many.
Looking over the medical records of 365,426 women 40 to 74 years old who underwent 831,455 mammograms from 2002 to 2011, the authors tried to determine what factors most accurately predicted the chances of a woman developing an invasive cancer in the 12-month period after a negative mammogram; in other words, interval cancers that may have caught if the woman in question had undergone more testing in addition to their annual mammogram. These factors included breast density as well as the percent risk of a woman developing cancer in the next five years, an equation calculated by determining the age, race, and family history of the woman, among other criteria.
They concluded it was only those with a five-year cancer risk of over 1.67 percent and extremely dense breasts (21 percent of women with dense breasts), or a five-year risk of over 2.5 percent and heterogeneously dense breasts (24 percent of dense-breasted women) who were at high risk of developing an interval cancer. The chances of advanced cancer were highest among those with either heterogeneously or extremely dense breasts and over 2.5 percent five-year risk. But contrary to popular belief, high breast density oftentimes didn’t correlate with a high five-year risk; more than half of women with heterogeneously and extremely dense breasts had a low to average five-year risk.
These results matter a great deal for the approximately half of American women with dense breasts. Should the study's findings hold up, it would mean that only 24 percent of women with dense breasts truly benefit from additional screening. The authors also found that women with dense breasts but a low 5-year risk are currently being subjected to an unacceptably high rate of false positive results on mammograms, in part because doctors believe that dense breasts are a more crucial risk factor than they actually are. "Breast density should not be the sole criterion for deciding whether supplemental imaging is justified because not all women with dense breasts have high interval cancer rates," the authors concluded.
As the authors admit, cancer screening is a complex balancing act. They theorize that additionally screening 100,000 women with dense breasts would catch 89 interval cancers, while screening the two highest risk groups (24,294 women) would catch 35 cancers, yet the authors recommend the former method. That might seem like a callous decision to make, but the time, effort, radiation risk, and emotional turmoil involved in making 75,000 women go through unnecessary testing shouldn’t be ignored, they note.
With only so many hours in the day or radiologists assigned to a lab, it’s important that our public health policies be guided by both compassion and effectiveness. In this case, that might mean discarding our long-held beliefs about certain breast cancer risks.
Source: Kerlikowske K, Zhu W, Tosteson A, et al Identifying Women With Dense Breasts at High Risk for Interval Cancer: A Cohort Study. Annals of Internal Medicine. 2015



























