Obesity May Be Influenced By Gut Bacteria, And Researchers Are Closer To Understanding How
The theorized connection between the trillions of bacteria that call our guts home and conditions like obesity has steadily become more concrete over time.
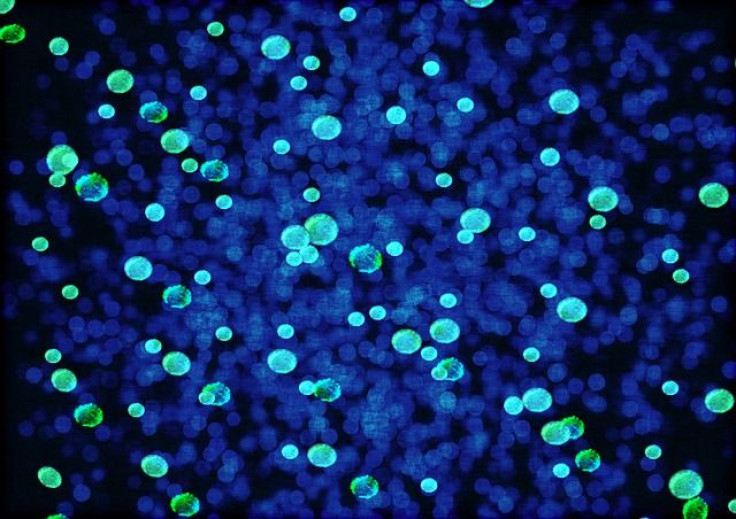
Studies have found that a diet high in fat, a common risk factor of obesity, can trigger widespread disruptions to the microbial environment, or microbiota, in test animals like mice and zebrafish. Others, meanwhile, have showed that this link works both ways: When scientists transplanted gut bacteria from a group of healthy mice into a group of mice engineered to have no bacteria whatsoever, the lean germ-free mice became fatter. This same effect was seen even when the gut bacteria from obese people was transplanted into these mice.
For the most part, though, we’re still largely in the dark as to how this relationship actually operates. Without understanding this crucial piece of the puzzle, it’ll be impossible for us to ever manipulate the connection to our benefit in order to prevent or treat obesity. A new mouse study published Wednesday in Nature, however, may shine a light on where to look.
A High-Fat Trigger
Senior author Dr. Gerald Shulman, co-director of the Yale Diabetes Research Center, told Medical Daily that he and his colleagues had embarked on a series of experiments that were meant to follow up on a mouse study of theirs published the year before. This study found a distinct link between insulin resistance, a risk factor of both Type 2 diabetes and obesity, and increased levels of the chemical acetate, which is part of a motley crew known as short-chain fatty acids (SCFAs). For their new study, they wanted to trace how and why this happened.
After examining insulin-resistant mice fed high-fat diets for up to four weeks, they found that these mice had much more acetate in their bodies than mice that were on a normal diet. All this acetate then promoted the increased secretion of insulin from the pancreas (triggered by higher levels of sugar in the blood) as well as increased levels of the hunger hormone ghrelin. The researchers said this process was likely activated through the parasympathetic nervous system, which consists of specialized nerves that help regulate unconscious body processes like salivating, sexual arousal, and digestion.
Theorizing that the gut bacteria of the high-fat mice had gorged on the food and produced acetate, they mucked around with the mice’s digestive systems — by cutting out their entire colon for instance. Once done, acetate levels dropped back down to around normal. In two other experiments, the researchers also saw gut bacteria produce acetate when cultured in the lab, and when they treated droppings from these mice with broad-spectrum antibiotics, they saw a marked drop in acetate production.
All of these experiments strongly suggested that the gut microbiota, fueled by a high-fat diet, was the main source of acetate production in the mice, the authors wrote.
Shulman and his colleagues were also able to create a positive feedback loop; by constantly infusing their hapless mice with acetate for 10 days straight, they effectively turned the mice into obese eating machines. In other words, the mice secreted more insulin and ghrelin because of the acetate, which then led to increased hunger and food intake, and ultimately to insulin resistance, weight gain, and other metabolic problems. All the added food only pumped more acetate into the system, which started the loop all over again.
In people, this same loop might be seen when they constantly eat a high-fat diet — the diet gradually changes the landscape of their gut microbiota to favor acetate-producing bacteria, which then makes people eat more food. Then, the cycle repeats.
“Together, these findings identify increased acetate production resulting from a nutrient-gut microbiota interaction and subsequent parasympathetic activation as possible therapeutic targets for obesity,” the authors wrote.
Of course, obesity and its related conditions are a multifaceted problem, caused by a complex and sometimes contradictory mix of factors. Other SCFAs, like butyrate — produced when our gut bacteria digest fiber — have shown the ability to protect against the development of obesity. And while a high-fat diet is known to promote the growth of the bacterial species Firmicutes while decreasing levels of Bacteroidetes (including in the current study), we still don’t know whether resculpting our gut microbiotas will stop the loop dead in its tracks. That said, some early evidence has shown that obese people given fecal transplants from lean donors go on to experience positive changes in their metabolism.
Shulman's team now plans to test whether its results can be replicated in people.
Source: Perry R, Peng L, Barry N, et al. Acetate mediates a microbiome–brain–β- cell axis to promote metabolic syndrome. Nature. 2016.



























