Too Much Iron In The Brain May Lead To Parkinson’s Disease, Damages Neurons
Researchers have known for some time that too much iron buildup in the brain is associated with Parkinson’s disease, as well as other neurodegenerative diseases. Excess iron can be measured through a person’s teeth, providing clues about their exposure to iron and its link to these diseases.
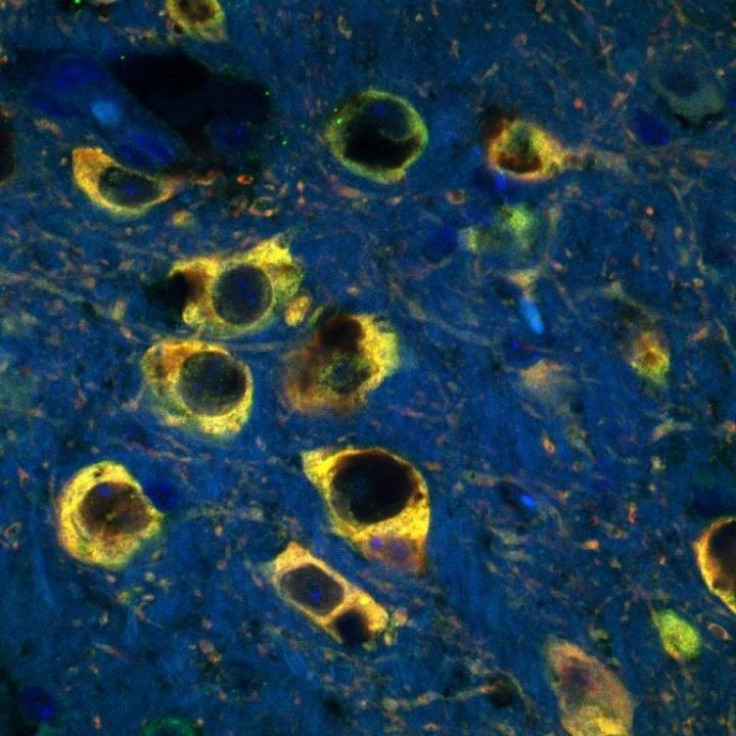
A new study examines the link more deeply in an attempt to understand why iron contributes to Parkinson’s disease. Researchers from the Andersen lab at the Buck Institute for Research on Aging found that excess iron damages neurons in the brain by impairing lysosomes, structures in cells that break down and repair harmed proteins.
Parkinson's disease is a neurodegenerative disease that affects the central nervous system, impairing movement and causing tremors. Some 200,000 people in the U.S. suffer from Parkinson's every year, and it can't be cured — many of the factors underlying the disease are still poorly understood. Researchers believe that genetics and environmental factors may play the largest role in the development of the disorder, but the latest study examines how excess iron may be involved in the mix.
Lysosomes are involved in a process called autophagy — a way for cells to break down damaged proteins, then rebuild them into new proteins. Autophagy has been shown to play a role in various physiological issues, particularly aging and neurodegenerative diseases like Alzheimer’s. As people age, lysosomes begin to slow down, impairing this recycling process and causing bad proteins to build up inside cells — and ultimately allowing excess iron to enter the neurons, causing toxic oxidative stress.
“It’s recently been realized that one of the most important functions of the lysosome is to store iron in a place in the cell where it is not accessible to participate in toxic oxidative stress-producing reactions,” Julie Andersen, a senior scientist at the Buck Institute and an author of the study, said in the press release. “Now we have demonstrated that a mutation in a lysosomal gene results in the toxic release of iron into the cell resulting in neuronal cell death.”
The researchers focused on a rare form of Parkinson’s known as Kufor-Rakeb syndrome, which is an early-onset version of the disease that appears as early as the adolescent or teen years. Kufor-Rakeb is associated with a mutation in the ATP13A2 gene, so researchers removed that gene in mice and cultured human dopaminergic cells. They found that when the gene was removed, the lysosomes in the cells couldn’t maintain the balance of iron in the cells.
“Mutations in this same gene have also been recently linked to sporadic forms of [Parkinson’s disease],” Andersen said in the press release. “This suggests that age-related impairments in lysosomal function that impact the ability of neurons to maintain a healthy balance of iron are part of what underlies the presentation of PD in the general population.”
Of course, iron and impaired lysosomes may not be the only factors behind the development of Parkinson’s disease. Recent research posits that Parkinson’s may be caused by overactive cells that overheat and burn out, and other studies have linked depression to an increased risk of Parkinson’s. But Andersen believes her latest study is significant in understanding the association between iron and Parkinson’s, as well as the link between oxidative stress and neurodegeneration.
Source: Andersen J, et al. Regulation of ATP13A2 via PHD2-HIF1a Signaling is Critical for Cellular Iron Homeostasis: Implications for Parkinson’s Disease. The Journal of Neuroscience, 2016.



























