Patient Stem Cells Help Researchers Pinpoint New Treatments For Cognitive Decline: Dementia In A Dish?
Alzheimer's disease and other forms of dementia are debilitating disorders that affect a large number of the world population. And despite the Obama administration having pledged hundreds of millions of dollars to Alzheimer's research in recent years, not much progress has been made to halt the disease that is believed will affect nearly 16 million people by 2050.
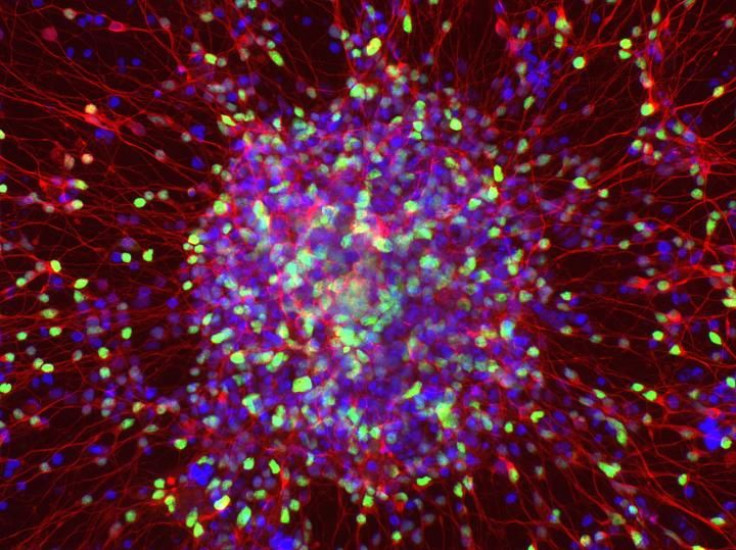
Now, new research offers light onto how these degenerative diseases develop. Through the use of stem cells, Belgian researchers have produced a form of “dementia-in-a-dish” in the lab and managed to look more deeply into how the disorder develops and maims neurons in the brain.
Deriving skin cells from three patients, the researchers developed them into embryonic-like stem cells. These pluripotent stem cells are able to turn into any type of cell — which is quite useful in studying diseases. In this case, the researchers developed the stem cells into the kind of neurons that are most often affected by frontotemporal dementia (FTD), known as cortical neurons. FTD is a group of disorders caused by progressive cell degeneration in the frontal lobes of the brain (which are located behind your forehead), or the temporal lobes (which are located behind the ears), according to the Alzheimer’s Association. Through the damaging of neurons, people with FTD often begin gradually experiencing language or emotional disorders.
Published in the journal Stem Cell Reports, the study has potentially found a new treatment strategy for dementia-related diseases. “Use of induced pluripotent stem cell (iPSC) technology makes it possible to model dementias that affect people later in life,” Catherine Verfaillie of KU Leuven, senior author of the study, said in the press release.
Dementia is an umbrella term for various disorders associated with mental decline and aging, such as Alzheimer’s disease and vascular dementia. More than five million people in the U.S. are living with the disease, and about 500,000 people die per year due to Alzheimer’s disease. However, there is still no cure for dementias.
Induced pluripotent stem cell technology, known as iPSC for short, gives researchers a more effective view into how this disease (and plenty of others) develops and works. In this particular study, Verfaillie and her colleagues took induced pluripotent stem cells (iPSCs) from three different patients who carried a mutation in a gene called progranulin (GRN). This gene mutation is often linked to frontotemporal dementia. The iPSCs turned into cortical neurons, which were shown to be impaired from the mutation and thus related to frontotemporal dementia.
Previous studies have used the iPSC technique to study dementias and other neurological disorders. A University of Cambridge paper published in 2014 notes that despite some challenges with the iPSC technique, these studies “are encouraging for the utility of stem cell systems for both modeling and understanding the cell and molecular biology of dementia in human neuronal systems.”
In the most current study, the researchers were able to pinpoint a new track for treatment for dementia patients. “iPSC models can now be used to better understand dementia, and in particular frontotemporal dementia, and might lead to the development of drugs that can curtail or slow down the degeneration of cortical neurons,” Verfaillie said in the press release.
One pathway, known as the Wnt signaling pathway, which is involved in neuronal development, is often impaired in people who have frontotemporal dementia. The researchers found that genetic correction of the Wnt signaling pathway led to the iPSCs to turn into regular, healthy cortical neurons; perhaps this may be a new form of treatment if further examined.
“Our findings suggest that signaling events required for neurodevelopment may also play major roles in neurodegeneration,” Philip Van Damme, who works at the Leuven Research Institute for Neuroscience and Disease and was also a senior author of the study, said in the press release. “Targeting such pathways, as for instance the Wnt pathway presented in this study, may result in the creation of novel therapeutic approaches for frontotemporal dementia.”



























