Rare Immune Deficiency Disorder WHIM Syndrome Sees 'Spontaneous Cure' With Major Chromosome Deletion
By all accounts, it was a catastrophe that turned into a cure. In 1964, an American hematologist named Wolf Zuelzer encountered a young patient suffering from a never-before-seen immunodeficiency disorder. She had warts, infection, and a severe lack of circulating white blood cells, known as leukopenia. Zuelzer didn’t know what to call it.
Some years later — the actual timeline is still fuzzy to scientists — when the woman was in her 30s, the condition randomly subsided. Her symptoms vanished. In the time since her initial diagnosis, doctors had come up with a title for the rare disorder: WHIM syndrome, named for its characteristic warts, hypogammaglobulinemia, infections, and myelokathexis. The disorder is so rare, researchers estimate it affects only 60 people worldwide, and new evidence says the cure is out there.
Out Of Thin Air
One of the most ruinous bodily processes involves the total rearrangement and deletion of a person’s chromosomes. The phenomenon is called chromothripsis, or “chromosome shattering.” Entire pairs disintegrate into pieces, switch places, and reassemble themselves into random and chaotic positions, with hundreds of gene alleles getting forever lost in the shuffle.
“You might imagine someone making a quilt,” said Dr. Philip Murphy, who heads the Laboratory of Molecular Immunology at the National Institutes of Health. “You take fabric, tear it up into pieces, take the ones you like, and put them together in a newer arrangement.” Most of the time what results isn’t a beautiful mosaic that works as one unit. But in the female patient’s case, chromosome shattering is precisely what the doctor ordered.
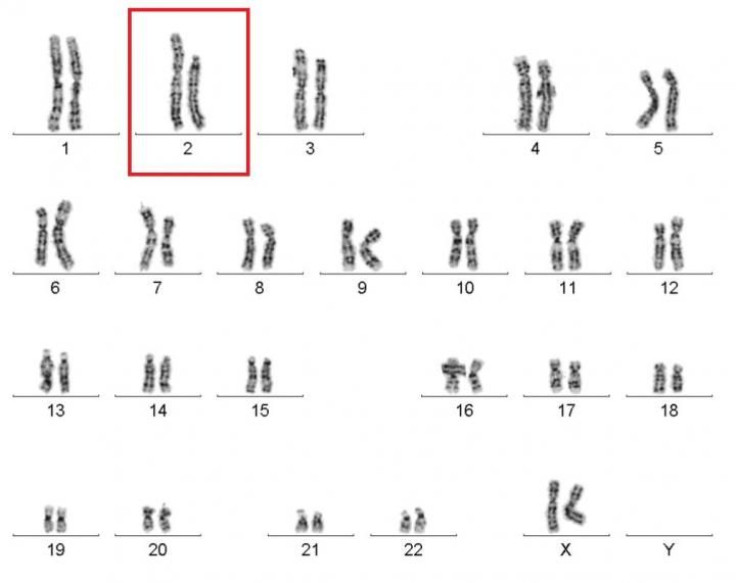
In 2003, a group of researchers found WHIM syndrome stems from mutations of CXCR4 gene, an allele located on chromosome 2. When Murphy and his team looked at the patient’s genetic makeup, they found 164 total gene deletions. CXCR4 was one of them.
“Putting all the pieces together, we think that what happened was in her thirties, one of her stem cells in her blood underwent chromothriptic event and that deleted her disease gene CXCR4,” Murphy told Medical Daily. That event did two things. First, it transformed the unhealthy WHIM cell into a healthy non-WHIM cell. But the event didn’t just kill the unhealthy cells, Murphy pointed out. “It basically outgrew the WHIM stem cells that were in her bone marrow and repopulated her bone marrow with the non-WHIM cells.”
Once the patient had those new cells, her immune system returned to a normal state. Her warts disappeared and the infections stopped — all this after 30 years of non-stop expression. “So it sounds kind of crazy and farfetched,” Murphy said, “but that’s actually what happened.”
Future Transplants
Prior to the recent findings, chromothripsis had yielded devastating results in all cases. Now evidence on the contrary exists. While nothing is written in stone, the research team is anxious to explore what else stem cells are capable of repairing.
“There’s a subtext to this,” Murphy said. Since they found a way to deliberately transplant the disease CXCR4 gene in stem-cell mouse models, this suggests the same methodology may apply to any and all cases where a transplant, or engraftment, would be used. These include gene therapy, cell therapy, and really “any context where you are putting cells in and hoping they’ll engraft in the bone marrow and take over.”
Murphy says he’d also add one other point of interest to the study, which may help move the inexplicable and otherworldly into the realm of reality. “Doctors have all heard of patients termed ‘miracle cures,’” he said, “and now I think anyone who has a patient like that should consider looking for chromothripsis as a potential natural explanation for the miracle. I think that’s one important thing that falls out of this research.”



























