Simple Blood Test Could Detect Advanced Skin Cancer, Offer Quick Treatment
As difficult as it is to treat melanoma — the most dangerous kind of skin cancer —detecting it in the first place can be just as laborious. But that could change in the near future, as researchers from the University of Dundee claim to have devised a simple blood test that identifies elevated levels of a certain gene in patients’ DNA that they say could be the key to stopping the disease in its tracks.
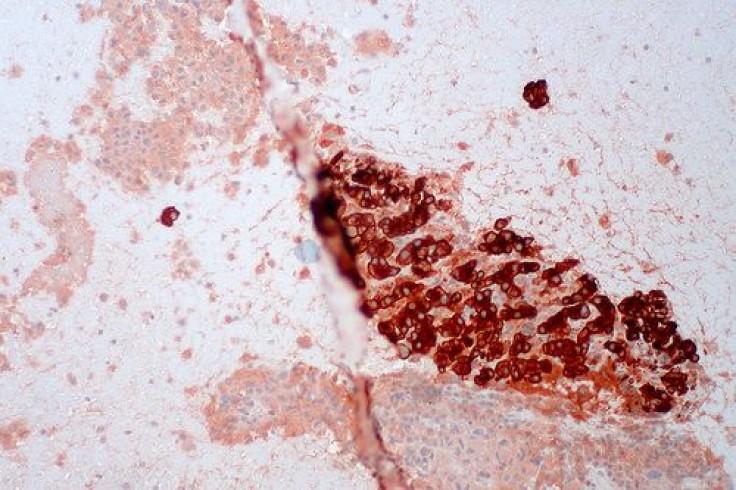
Skin cancer is the most common form of cancer in the United States, and melanoma is the deadliest of skin cancers. According to the Centers for Disease Control and Prevention, 61,061 people were diagnosed with melanomas in 2010. Of those, 9,154 died. Melanomas are relatively rare; basal cell cancers, on the other hand, are the most common and also the easiest to cure. Researchers now claim they have discovered a straightforward test that identifies to what extent the more dangerous forms of skin cancer have spread. The research team presented their findings at a recent conference for the National Cancer Research Institute.
"By using a blood test, we have the basis of a simple and accurate way of discovering how advanced the disease is, as well as an early warning sign of whether it has started to spread,” Dr. Tim Crook, study author and consultant medical oncologist at the University of Dundee, told the BBC. "This would give doctors and patients important information much sooner than is possible at the moment.”
Crook and his colleagues pinpointed the TFP12 gene in patients’ DNA as the key marker for melanoma spread. Doctors usually speak of genes being either “switched on” or “switched off.” When the TFP12 gene is switched on, it helps regulate the production of healthy skin cells. But in the presence of chemical “tags,” through a process known as DNA methylation, the gene gets switched off. Doctors performing the study found that greater levels of methylation indicated the cancer was more diffuse in the body.
"There's increasing evidence that the latest treatments are more effective in these early stages and, if we can identify patients whose cancer has only just started to spread, this would significantly improve the chances of beating the disease,” Crook said.
Dr. Charlotte Proby, a dermatologist based at the University of Dundee, echoed Crook’s sentiments, adding that blood tests are a simple, yet elegant and effective way to map the landscape of DNA underneath the skin. The research team at the University has also found the gene NT5E to play a potential role in forestalling the spread of aggressive melanoma.
The ultimate objective, as Proby sees it, is developing a robust arsenal of biomarkers that can be deployed when treating a patient’s cancer, so that any flaws in treatment aren’t the result of a poor understanding of the disease itself. "Our goal,” she said, “is to develop a panel of similar biomarkers that will help us to accurately detect those patients needing extra treatment to fight their melanoma.”



























