Sleep Apnea And Alzheimer's Disease Connected, Study Finds
Lean people with sleep-disordered breathing (SDB) are more likely to have certain biomarkers of the early stages of Alzheimer's disease (AD), a new study shows.
The study, led by Dr. Ricardo S. Osorio of New York University, contributes to a sparse but growing body of evidence that the two conditions are related.
Study participants included 68 cognitively normal elderly patients, ages 64-87. Researchers observed the subjects for two nights of home monitoring for sleep disordered breathing and tested for diagnostic indicators of Alzheimer's disease. Participants were considered to have sleep-disordered breathing if they experienced at least 5 episodes (lasting ten seconds or longer) of shallow or no breathing per hour while they slept.
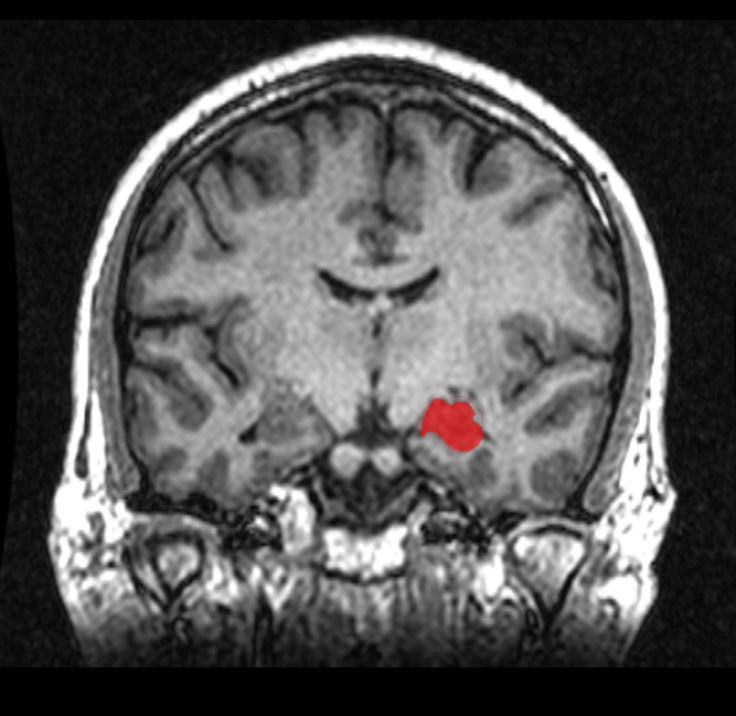
Osorio found that a relationship appeared to exist between biomarkers for AD and sleep-disordered breathing, but mainly among lean patients (those with a body mass index of < 25 kg/m2). In lean patients, the severity the SBD correlated to the amount of P-Tau protein found in the cerebrospinal fluid. Tau proteins have been observed to form abnormal deposits in the brain associated with Alzheimer's disease. Lean patients with SDB, compared to lean patients wthout SDB, also had smaller hippocampi, a region associated with memory storage.
Researchers also found that lean patients with SDB had reduced glucose metabolism in certain AD-vulnerable regions of the brain, including the medial temporal lobe — a region involved with long-term memory — and the posterior cingulate cortex or precuneus. Though the function posterior cingulate cortex is unknown, lower levels of metabolism in the region are observed in people with AD.
Obese patients (those with body mass index > 25 kg/m2), glucose metabolism was reduced in the medial temporal lobe, but no other significant changes in biomarkers was found.
The biomarkers used in the study are not currently used to diagnose Alzheimer's disease clinically. Rather, they are signs that have appeared while researching non-symptomatic people who later develop mild cognitive impairment and dementia due to Alzheimer's disease.
"Our study did not determine the direction of the causality, and, in fact, didn't uncover a significant association between the two, until we broke out the data on lean and obese patients," Osorio said.
Determining whether one condition causes the other is the next item on Osorio's research agenda. He and his colleagues propose a two-year longitudinal study in which patients would be given a continuous positive air pressure (CPAP) machine to treat their sleep apnea. Biomarkers for AD will be measured before and after, to see if the CPAP treatment will have any effect.
"If they don't change, the probable conclusion is that these patients are going to develop AD with or without CPAP, and that AD may either be causing the apneas or may simply coexist with SDB as part of aging," Osorio said.
Both the prevalence of AD and sleep apnea skyrocket in later ages. Alzheimer's disease http://www.alz.org/downloads/facts_figures_2012.pdf" target="_blank">affects 13 percent of people age 65 and older and nearly half of people 85 and older. An estimated 10-20 percent of middle-aged adults and 30-60 percent of those over 65 have sleep-disordered breathing.
Findings will be presented at the American Thoracic Society 2013 International Conference.



























