Spinal Cord Injury Repair To Borrow Nerve Regeneration Mechanism In Lower Animals
Scientists from the Salk Institute are working on perfecting a molecule that convinces damaged nerves to regrow following spinal cord injury. A new study suggests the tiny shift, which happens naturally among whales, snails, frogs, and dogs, could lead to major breakthroughs in treating victims of severe nerve damage.
While more advanced from an evolutionary point of view, humans and primates fall oddly behind when it comes to self-repairing injuries located on individual nerve cells. The new findings present a model for interrupting the body’s normal processes to produce a similar effect of those found organically in lower animals. If lab tests can transfer to human models, scientists would have the ability to offer people with paralysis and spinal cord injuries a new chance at mobility.
"This research implies that we might be able to mimic neuronal repair processes that occur naturally in lower animals, which would be very exciting," said Salk professor and the study's senior author Kuo-Fen Lee.
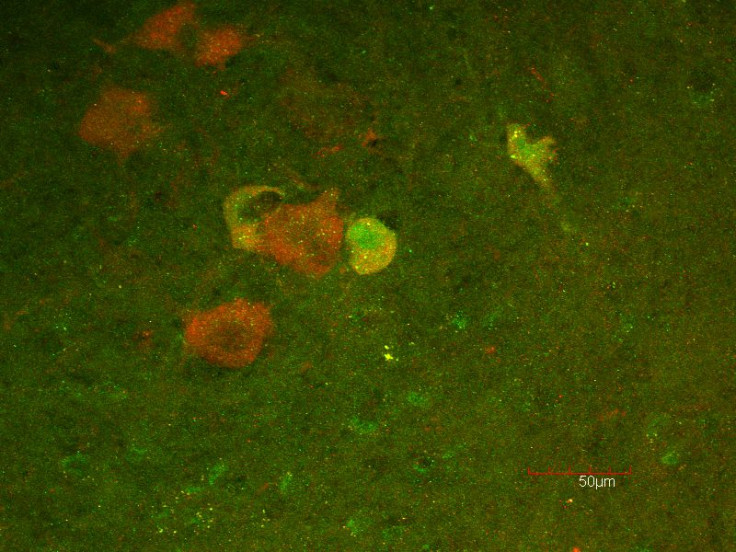
Key to the research team’s study was a group of protective sheaths, called myelin, surrounding the axons that extend from neurons. Axons are long, tail-like structures that emit a signal to other cells. Without their signaling power, nerves effectively die.
In prior research, Lee and his team found a specific protein, called p45, was responsible in certain animal models for jumpstarting nerve regeneration, and it did so by preventing the myelin from slowing things down. Humans, however, don’t carry p45. We use a separate protein called p75. Unfortunately for us, p75 does the exact thing we’d like to avoid — that is, promote myelin’s disruption of nerve regeneration.
"We don't know why this nerve regeneration doesn't occur in humans,” Lee admitted. “We can speculate that the brain has so many neural connections that this regeneration is not absolutely necessary.” However, the true reason remains a mystery. The best scientists like Lee can do is to intervene with tools they borrow from other species.
In their current study, the research team looked at how a pair of p75 proteins bind together to latch onto the inhibitors released from damaged myelin. Examining the relationship under nuclear magnetic resonance technology, they discovered that introducing p45 proteins tore apart the paired molecules. Even more impressive, they were able to bind to the initial myelin site, preventing new p75 from joining in, and allowed the axons to regrow.
"For reasons that are not understood,” Lee said, “when p45 comes in, it breaks the pair apart.”
For future research, this means introducing p45 or a similar disruptive agent should help break apart the laggard p75 protein bonds, which weren’t all that welcome to the party in the first place. One tactic would be to swarm each damaged neuron with p45, though Lee suspects a smarter idea would be to use one small molecule to jam the link between the inhibitory p75 proteins, essentially blocking the blockage.
"Such an agent could possibly get through the blood-brain barrier and to the site of spinal cord injuries," Lee said. As for what’s next, he and his team are planning to test how well p45 can inhibit the negative effects of p75. "That is what we hope to do in the future.”
Source: Vilar M, Sung T, Chen Z, et al. Heterodimerization of p45–p75 Modulates p75 Signaling: Structural Basis and Mechanism of Action. PLOS Biology. 2014.



























