Sudden Cardiac Arrest Awareness Month Highlights Myths And Truths; Be A Heart Hero

Many of us take for granted the rhythmic and constant beating of our hearts, but what if there’s something wrong and we don’t even know it? During Sudden Cardiac Arrest Awareness month, the importance of screening hearts and educating the life-saving tools needed to ensure safety are emphasized. The Hypertrophic Cardiomyopathy Association (HCMA) is one of the leaders in spreading awareness with accuracy and creating tools for health organizations, schools, and workplaces.
Hypertrophic cardiomyopathy is a primarily genetic heart disorder, in which the muscle is abnormal. The condition affects one out of every 500 people and is the leading cause of sudden cardiac arrest. Although there are all forms of heart conditions, it’s important to understand there are serious differences between heart attacks and cardiac arrest. But as the HCMA founder and CEO Lisa Salberg says, “the outcome may be the same by ending up with a funeral, but they’re as different as night and day.”
People often mistake these terms, but a heart attack occurs when a blocked artery prevents oxygen-rich blood from reaching a section in the heart, and if not opened back up immediately, the artery begins to suffer and die. Unlike sudden cardiac arrest, the heart doesn’t stop beating during a heart. A sudden cardiac arrest occurs suddenly and without warning, triggered by an electrical malfunction in the heart that causes an irregular heart beat. When the blood pump is disrupted, the heart cannot move blood to the brain, lungs, and other organs, and death threatens the person within minutes.
“There's a whole school of thought that says we should have every kid lined up in America to test them,” Salberg told Medical Daily. “But the concept of community-based electrocardiogram screening isn’t the answer. One-third of the tests are wrong. You need a really skilled eye and image when you’re screening 1,000 kids at a time.”
Salberg recommends solidifying a relationship with your general practitioner and making sure they’re involved with their children’s heart health by knowing what to look at and asking the right questions about your family history. There is a common misconception that when trying to evaluate risk for genetic disorders such as HCM, you just need to look at your parents and grandparents health history. But ignoring the rest of the tree can be putting you and your children at risk.
“If I could impart one piece of advice to the general public, it would be to really understand your family history. The past is a peek at your future, and it’s a huge message that’s complicated to figure out not everyone has all of the death certificates and information they need. But we have to stop thinking of family trees as up, into our parents and grandparents’ history. You need to look over at aunts, uncles, and cousins. We need to look up, over, and then down at how it affects our children.”
Just this month, the American Heart Association and the American College of Cardiology released an updated list of key screening elements. The 14-point checklist has been circulated for doctors to familiarize themselves with congenital and genetic heart disease screening for young people between the ages of 12 and 25. If any of the points are checked off for positive, further testing will be needed. Salberg coauthored the screening recommendations and translated them into parent friendly-language for the HCMA’s risk assessment form in order for it to be more readily understood for parents who want to help ensure their child is safe and correctly evaluated.
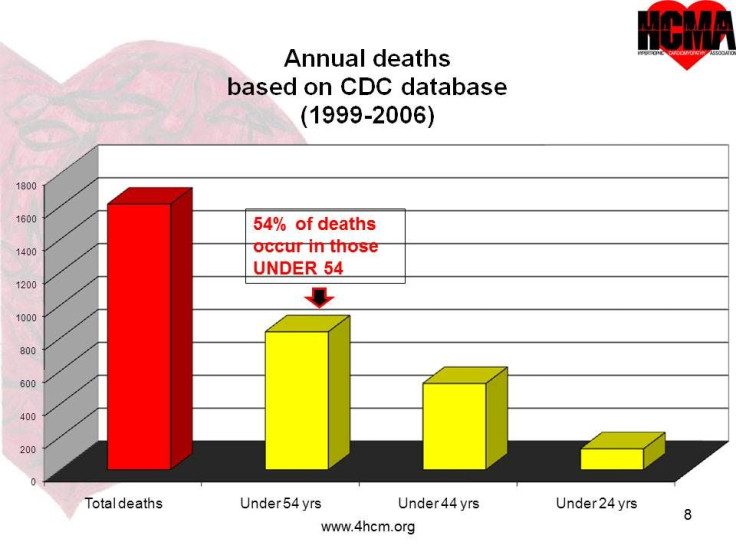
Many parents and the general public share a misconception that athletes are at greater risk for sudden cardiac arrest, which simply isn’t true. In fact, an average of 70 athletes die each year from this condition and that only accounts for 20 percent of the total number of people 24 years and younger who die every year. With a total of 80 percent of deaths occurring in non-athletes, the spotlight of concern should really be shifted to the entirety instead of focused on one group. Salberg does point out that people with HCM don’t handle adrenaline the same as someone with a normal, healthy heart, but it doesn’t necessarily put athletes at a higher risk.
That also doesn’t mean athletes aren’t important though. The HCMA designed a drill called the “Dr. Heart Drill” that are specifically designed guidelines on how to respond to a team sport emergency scenario. It’s important for students, athletes, coaches, and parents to all be on the same page if something goes awry because there’s only a small window of time to act in order to get the patient into the emergency room with as much of a healthy body as possible to aid in a smoother recovery. By ensuring there are AEDs and training programs for people in educational institutions, workplaces, and any public places, the risk could drop tremendously.
“We have done a very poor job as a nation at explaining the key screening elements to educating parents, teachers, coaches, and students,” Salberg said. “We are missing an amazing opportunity to save a lot of lives here.”



























