Treating Obesity Using Patient's Family, Community, And Clinical Services
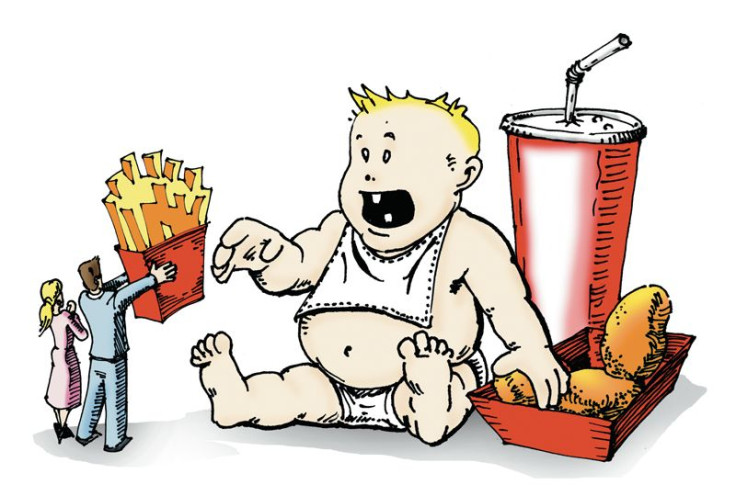
As YouTube user Nicole Arbour recently learned, fat-shaming does not work, regardless of how many bad jokes you pepper people with. In fact, among the innumerable weight loss and dieting tips that are introduced to the public each year, only a few have been considered successful. A new model proposed by researchers from the George Washington University Milken Institute School of Public Health could offer a universally effective way for treating and preventing obesity.
"This public health crisis calls for a transformation in the way we handle obesity, a chronic disorder that is fueling high rates of diabetes, heart disease, and cancer in the United States," said Dr. William H. Dietz, director of the Sumner M. Redstone Global Center for Prevention and Wellness at GW, in a statement.
Dietz and his colleagues feel that if a “radical change” is not made with the U.S. health care system and the environment, then the number of American adults struggling with obesity (79 million) will remain “unacceptably high.” They recommend a system centered around each individual patient and how they engage with health care providers and family members. Current weight loss paradigms that have been deemed successful emphasize behavioral changes — healthy food and physical activity — and family involvement.
This new model would also require that health care professionals adopt behavioral strategies used to help ease their transition into healthy dieting and exercise. Clinical services should accept standards that are sensitive to the stigma surrounding obesity while offering easier ways lose and maintain weight. One way of doing this would be partnering with community systems, like a local YMCA, which offer structured techniques for losing weight.
"We propose a new model for the prevention and treatment of obesity, one that integrates health care in the clinic with resources in the community that make it easier for people to prevent unhealthy weight gain or lose weight and keep it off," Dietz added.
Dietz stresses treating obesity for what it is: a complex biological condition. That would require policy changes, such as adding behavioral change strategies to training for health care professionals and easier access to up-to-date information regarding obesity treatment. Other policy changes would include more hospital involvement, payment methods that reward quality of care, and health plans that support environmental and social norm changes that facilitate weight loss.
Although the authors of this study do not expect this change to be made overnight, they do recognize support for their new model in current health standards. For example, they point out that the Affordable Care Act’s emphasis on prevention is in line with their model, but clearly there are challenges with implementing a new agenda. Namely the need for incentives given to a system that help its patients beyond the walls of a hospital, clinic, or any health care setting.
Source: Solomon L, Pronk N, Dietz W, et al. An Integrated Framework for the Prevention and Treatment of Obesity and Its Related Chronic Diseases. Health Affairs. 2015.



























