After 30 Years Of Cancer Overdiagnosis, Scientists Are Calling For A Redefinition Of The Disease
Who would have thought that advances in medical technology could potentially lead to unnecessary diagnoses and detrimental treatment plans? In March 2012, the National Cancer Institute held a meeting to evaluate the problem of cancer overdiagnosis, which occurs when harmless tumors are detected and treated as rigorously as harmful ones are, often leading to the demise or injury or patients.
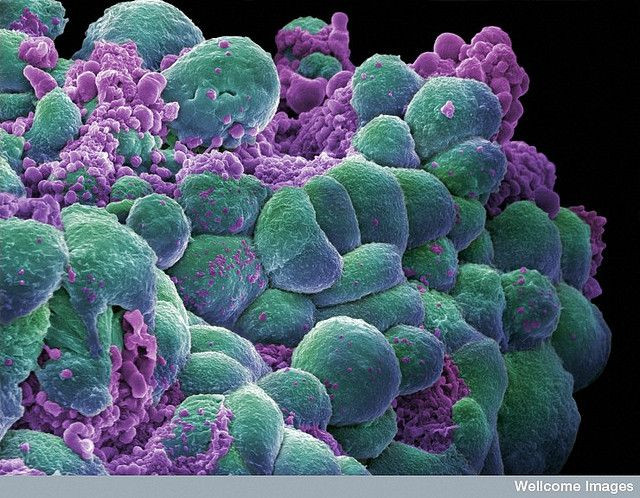
Cancer is merely an overgrowth of cells in a particular region, or organ, of the body. Upon diagnosis, patients tend to take the path of least resistance and opt for every possible treatment. But, a cancer diagnosis constitutes more than a few abnormal cells. The cells have to show the ability to continue to grow and cause the body harm. What's more, cancer treatments are highly invasive and can become debilitating, especially if they aren't needed. Thankfully, screenings for other cancers in the breast, lung, or thyroid will often pick up innocuous abnormalities that are misread as cancers.
Now, the acknowledgement by the National Cancer Institute — of cancer overdiagnosis and overtreatment — provides an opportunity to reshape cancer screening with a focus on redefining what cancer is and isn't.
"We need a 21st-century definition of cancer instead of a 19th-century definition of cancer, which is what we've been using," Otis W. Brawley, M.D., the chief medical officer for the American Cancer Society, told The New York Times.
The conference developed five suggestions for the National Cancer Institute to consider that were outlined in a new study:
1. Physicians and patients must recognize that overdiagnosis is common, even more so with frequent cancer screening
Given the sensitivity of cancer screening technology today, any cellular abnormality may be misunderstood as cancer. Overdiagnosis often occurs in areas of the body screened most often: breast, lung, prostate, and thyroid glands. Overdiagnosis can be prevented if more follow-up screenings are done, instead of starting treatment as soon as an abnormality is observed.
2. Lessen overdiagnosis
Related to acceptance of abnormal screenings, fewer unnecessary screenings should be performed. The convention suggests that only high-risk groups be screened for cancers vigilantly, with the goal of diagnosing actual cancers instead of innocuous abnormalities that will be fine if left untreated.
3. Change cancer terminology
The diagnosis of "cancer" should be reserved for when abnormalities in screenings are definitely found to be lethal and action against them becomes exigent. This means, new words are needed to describe non-urgent abnormalities, like "premalignant conditions" or "low risk lesions" to refer to benign lesions or cancer-like abnormalities seen, but which do not require immediate action.
"The terminology is just a descriptive term, and there's no question that has to be explained," said Dr. Larry Norton, the medical director of the Evelyn H. Lauder Breast Center at Memorial Sloan-Kettering Cancer Center. "But you can't go back and change hundreds of years of literature by suddenly changing terminology."
Norton indicates that cancer's definition will remain the same, but if descriptive terms are more specific, then proper treatments and therapies can be given to those who are in need and avoided by those who are not.
4. Create observational registries for low-risk lesions and abnormalities
Once differences between benign and malignant lesions are defined, other doctors screening for cancer need to be informed so that the new definition becomes the standard across the board. A registry will ensure that proper follow-up care is given to those who had abnormalities that do not need treatment now but may in the future. Similarly, if these definitions are disseminated as a standard, it will improve cancer care for everyone, including those who are diagnosed as having cancer.
5. Expand approaches to cancer progression and treatment
The Institute suggests that more research should be done regarding cancer treatment, disease management, and prevention.
Identification of these weaknesses in cancer research and diagnosis is promising. "This is a long way from the thinking 20 years ago when you found a cancer cell and felt you had a tremendous risk of dying," said Harold Varmus, M.D., the Nobel Prize-winning director of the National Cancer Institute. And as a result, diagnosis guidelines must change with the times.
Source: Esserman LJ, Thampson IM, Reid B. Overdiagnosis and Overtreatment in Cancer: An Opportunity for Improvement. JAMA. 2013.
Published by Medicaldaily.com



























