Bacteria And Blood Type Inexplicably Linked To Pancreatic Cancer, Researchers Continue To Investigate
The pancreas is a small, glandular organ located deep within the abdomen between the stomach and the spine. About six inches long, the pancreas secretes both enzymes and hormones that help with digestion and regulate the metabolism of sugars. Cancer of the pancreas, even when detected early, has a very poor prognosis with a high rate — 96 percent — of mortality. In fact, the National Cancer Institute estimates that new cases of pancreatic cancer will affect 45,220 (22,740 men and 22,480 women) while deaths from the disease may run as high as 38,460 in 2013.
Lifetime risk of this cancer is said to be one in 78; meanwhile, rates have slowly increased over the past decade. Very generally, men are 30 percent more likely to develop pancreatic cancer than women and African Americans are more likely to develop the disease than whites. Risk factors, established by scientific research, include tobacco smoking, chronic pancreatitis, obesity, and type II diabetes. Because these factors, collectively, account for less than half of all pancreatic cancer cases, researchers have long wondered what they might be missing.
Growing evidence indicates a link between pancreatic cancer and two different bacteria: a somewhat common strain found in the stomach and the strain that causes periodontal disease.
Spiral-Shaped Microorganism
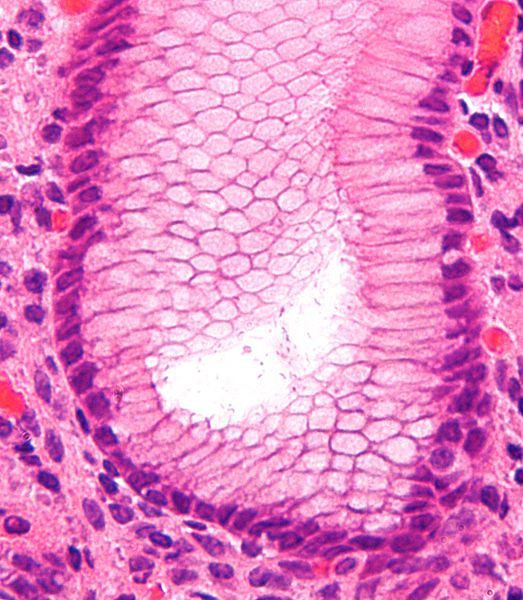
Helicobacter pylori, or H. pylori, is a spiral-shaped bacterium with flagella that produces urease, an enzyme that protects it from gastric acid. An H. pylori infection or colonization occurs when the bacteria begins to grow within and move around the liquid mucous layer of the stomach or when it adheres to the epithelial lining of the stomach. The Centers for Disease Control and Prevention (CDC) estimates that nearly two-thirds of the world's population harbors the bacterium; in the U.S. and other industrialized countries, the prevalence is about 30 to 40 percent, while in developing countries rates of infection may be as high as 70 percent.
Most people who have H. pylori infection remain unaware of it and never suffer symptoms — more than three-fourths of infections are asymptomatic — or develop illness from it, though it is known to cause most ulcers and gastric cancer. Spread of the bacterium may occur through contaminated food and water or through direct mouth-to-mouth contact, though this is not known for sure. Treatment of an H. pylori infection consists of a course of antibiotics; generally two varieties of antibiotics are prescribed at once, to help prevent the bacteria from developing a resistance to one particular antibiotic.
According to the CDC, gastric cancer, which is the second most common cancer worldwide, is more common in countries like China and Colombia, where H. pylori infects much of the population and does so in early childhood. Although a clear relationship between H. pylori and gastric cancer has been proven to exist, it has only recently been linked to pancreatic cancer — though not for everyone.
Blood Types
A research team from the Yale Cancer Center Prevention and Control Research Program examined the association between H. pylori, different blood groups, and risk of pancreatic cancer. Having reviewed the scientific literature, which includes studies showing an increased risk of pancreatic cancer for blood group A, blood group B, and blood group AB individuals when compared with blood group O individuals, the researchers hypothesized that the increased risk of pancreatic cancer from an H. pylori infection may be correlated with blood type. To test their theory, they conducted a population-based study of 373 case patients and 690 control subjects. The study was funded by the National Cancer Institute and approved by the State of Connecticut Department of Public Health.
"This study demonstrates an association between pancreatic cancer and H pylori colonization, particularly for individuals with non-O blood types," wrote the authors. "However, presence of the CagA virulence protein may temper the effect of H pylori on pancreatic cancer risk."
Scientists divide H. pylori strains into CagA (cytotoxin-associated gene A) positive or negative strains; the majority — upwards of 90 percent — of East Asian H. pylori isolates are positive while less, around 60 percent, of isolates in Western countries are found to be positive. In the study, then, the increased risk of pancreatic cancer was only associated with H. pylori when it was determined to be CagA-negative.
Along with increased investigation of H. pylori, scientists have also begun to further examine other bacteria, such as Porphyromonas gingivalis, to better understand how they might increase risk for the disease.
Oral Bacteria
The mouth is full of bacteria, mucous, and other particles. Bacteria cause inflammation of the gums or 'gingivitis' and untreated gingivitis progresses to 'periodontitis,' inflammation around the tooth. Specifically, Porphyromonas gingivalis has been identified as a cause of periodontal disease and, along with other bacteria, it can disseminate into the blood, stomach, heart, and even reach the brain. Once bacteria spread, the body's immune system responds and fights, and this may cause systemic inflammation.
Because of this response, scientists have begun to suspect that oral bacteria may be another contributing factor to pancreatic cancer. In a study conducted at Brown University, researchers analyzed data from the European Prospective Investigation into Cancer and Nutrition study. In particular, they measured the level of antibodies against P. gingivalis ATTC 53978 — a particular strain of the bacterium — in blood samples taken from 405 pancreatic cancer patients as well as blood samples taken from 416 'control' volunteers. (An elevated level of antibodies indicates the immune system has already begun to fight the strain.) They discovered that people with high levels of antibodies against P. gingivalis had a twofold higher risk of pancreatic cancer than individuals with lower levels of these antibodies.
"Periodontal disease might increase the risk for pancreatic cancer," wrote the authors. "Studies are needed to determine whether oral bacteria have direct effects on pancreatic cancer pathogenesis or serve as markers of the immune response."
Reseach, then, continues to advance toward a greater understanding of the bacterial causes of this most deadly cancer.
Sources: Michaud DS. Role of bacterial infections in pancreatic cancer. Carcinogenesis. 2013.
Michaud DS, Izard J, Wilhelm-Benartzi CS, et al. Plasma antibodies to oral bacteria and risk of pancreatic cancer in a large European prospective cohort study. Gut. 2012.
Risch HA, Yu H, Lu L, Kidd MS. ABO Blood Group, Helicobacter pylori Seropositivity, and Risk of Pancreatic Cancer: A Case-Control Study. Journal of The National Cancer Institute. 2009.



























