Blood Test For Childhood Germ Cell Cancers Can Detect Malignant Tumors Better Than Other Methods
Every year, 15,700 children are diagnosed with cancer. Though nearly 90 percent of them will survive, about one in 30 of these kids will be diagnosed with a rare cancer like meningioma — a rare brain tumor. Diagnosing these rare cancers can be difficult, but new research from the University of Cambridge and Addenbrooke's Hospital has found a non-invasive and affordable blood test could help detect them.
The test targets germ cell cancer, which develops in sperm and egg cells, and develops into both malignant and benign tumors in the testes and ovaries. Sometimes, however, these germ cells get trapped in a different parts of the body — like the brain — during embryonic development and turn into a tumor there. The overall survival rate for those with high-risk malignant germ cell tumors is below 50 percent, which makes accurate diagnosis and monitoring all the more important to those who are affected.
These diagnostic and monitoring methods are both expensive and imperfect, however. A biopsy, currently the most reliable diagnostic method, is also the most invasive; doctors surgically cut off a piece of the tumor, which is subsequently analyzed by a pathologist. Biopsies aren’t always accurate; sampling errors can lead to a misrepresentation of the tumor as a whole, which in turn gives doctors the wrong impression of the condition. CT and MRI scans, meanwhile, provide limited information, like where the tumor is. Because they can’t differentiate between a malignant and benign tumor, they’re not suitable for diagnoses. Moreover, they also expose the child to exorbitant amounts of radiation — children are already more sensitive to the effects.
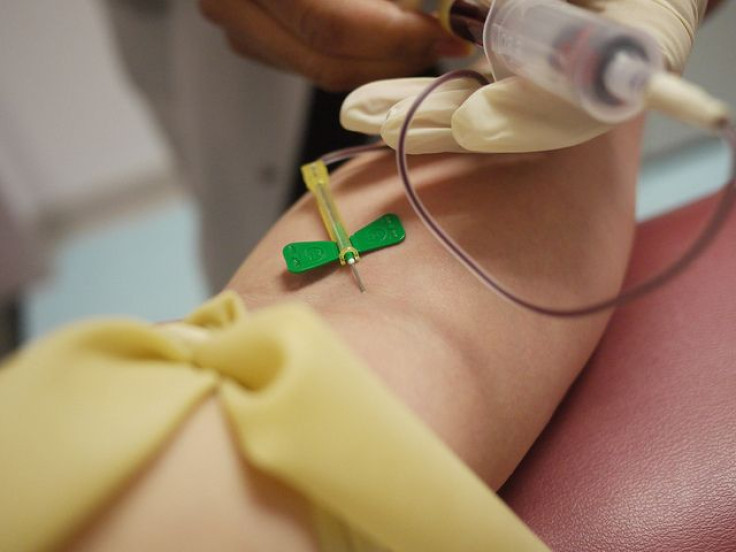
To circumvent these inaccuracies, prevent radiation exposure, and provide a more cost-effective solution, the researchers used 45 blood and cerebrospinal fluid samples from 25 patients for their tests. In both types of samples, the researchers looked for four specific pieces of microRNA — short genetic code clusters found in bunches in malignant germ cell tumors – that would tell them if a malignant tumor was present.
The researchers found their test was better at differentiating a malignant germ cell tumor from a benign germ cell tumor than a biopsy, and that it could find these anywhere in the body. What’s more, the test could also be used to determine how effective treatments are, as its cheap price meant it could be done several times when compared to biopsies and scans.
"Although relatively rare, childhood germ cell tumors need to be diagnosed accurately and followed up carefully to give us the best chances of treating them," said Professor Nick Coleman, from Cambridge’s Department of Pathology, in a press release. "At the moment, we are not good enough at diagnosing these tumours and monitoring their treatment; we need better, safer, and more cost-effective tests."
Other researchers have also created more cost-effective blood tests for diagnosing cancer. However, these tests only identify three out of every five malignant germ cell tumors, while the researchers’ tests were able to accurately identify a malignant tumor four out of every five times. This causes delays in diagnoses, which in turn affects the speed with which patients in need of urgent care get surgery. Of course, this just means further research will be necessary to ensure patients can get the most accurate, cost-effective treatment.
Source: Coleman N, et al. A pipeline to quantify serum and cerebrospinal fluid microRNAs for diagnosis and detection of relapse in paediatric malignant germ-cell tumours. British Journal of Cancer. 2015.



























