Brain Activity Linked To Metabolism: Ancient Greeks Knew Fasting Reduces Epileptic Seizures, Now Doctors Know Why
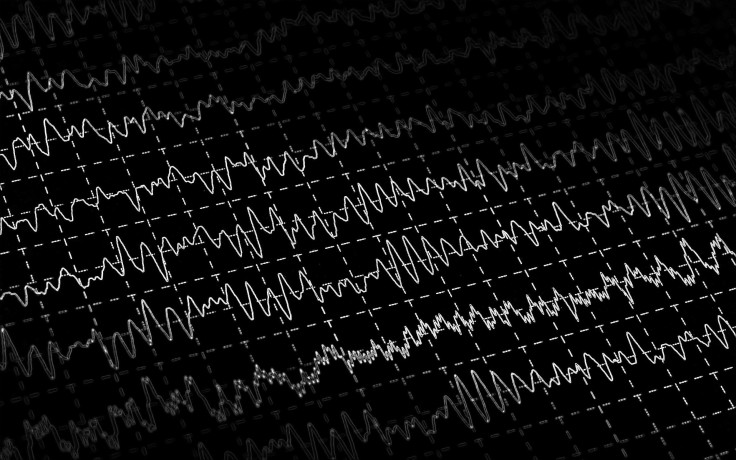
Researchers have discovered why certain diets are effective in treating epilepsy by finding that the metabolism of certain types of brain cells affects their ability to signal information. The connection between these two cellualr processes, which were previously assumed to be unrelated, opens up a potential avenue for treating epilepsy without the need for unpleasant medications.
Long before anticonvulsant drugs were made available in the 1950s, epileptics would linit their diet as a way to control seizures. Ancient Greeks noticed that periods of fasting would cause seizures to become more infrequent and less severe, while the Bible mentions fasting as an effective treatment. In the early 1900s, many epileptic patients resorted to the so-called ketogenic diet, which is high in fat and low in carbohydrates, because it was thought to mimic the physiological effects of fasting. Scientists have confirmed that these dietary restrictions somehow trigger biochemical changes that short circuit parts of the brain causing the seizures. But the mechanism underlying this therapeutic effect has remained a mystery.
In the current study, which was published in Nature Communications, the authors took a close look at neurons that inhibit activity since drugs that treat epilepsy function by strengthening the brain’s ability to step on the breaks before it crosses a threshold that makes it lose control. But as research leader and co-author, Dr. Derek Bowie of McGill University, explained in a press release, “These pharmacological approaches can have their drawbacks since the patients often complain of unpleasant side effects.” Furthermore, the authors pointed out that 20 to 30 percent of epilepsy patients don’t respond to drugs, which might explain why the ketogenic diet has become increasingly popular again.
Bowie and team made better sense of why this diet is effective by finding that a small chemical messenger acts as a go-between within inhibitory brain cells. Specifically, this chemical, called reactive oxygen species (or ROS), bridges parts of the cell that churns out energy with the mechanism that’s responsible for spreading epileptic activity to other cells. The authors were surpsied at this since it means that ROS plays an important role in healthy brains in addition to its infamous involvement with age-related neurological disorders, such as Alzheimer’s and Parkinson’s diseases.
Overall, the study shows that the brain already has an inbuilt remedy for dealing with over-activity that can be harnessed with the right kind of dietary jump-start. “Since our study shows that brain cells have their own means to strengthen inhibition,” Bowie explained, “our work points to potentially new ways in which to control a number of important neurological conditions including epilepsy.”
There has been a longstanding assumption that fasting and the ketogenic diet reduce seizures by affecting the same mechanism. But research is increasingly proving that these two strategies actually operate differently and thus can be used in tandem to better control seizures. This is particularly relevant for children who have epilepsy. Pediatric neurologists, such as Adam Hartman of Johns Hopkins Children’s Center, anticipate periodic fasts will be an alternative stand-alone therapy in children with drug-resistant epilepsy but warn that fasting needs to be done under strict supervision of a doctor.
Source: Accardi M V, Daniels B A, Brown P et al. Mitochondrial reactive oxygen species regulate the strength of inhibitory GABA-mediated synaptic transmission. Nat Commun. 2014.



























