Chronic Fatigue Patients Suffer 3 Major Brain Abnormalities; Findings May Lead To Clearer Diagnosis
The incessant fatigue characterized by chronic fatigue syndrome (CFS) that affects between one and four million Americans is often quite difficult to diagnose. But a new study, which found three distinct differences between the brains of patients with CFS and those of healthy people, promises to revolutionize diagnosis and provide insight into the underlying mechanisms of the condition.
"CFS (Chronic Fatigue Syndrome) is one of the greatest scientific and medical challenges of our time," said Dr. Jose Montoya, from the Stanford University School of Medicine, in a press release. His words, in effect, summarize the difficulty doctors face in diagnosing CFS, which is often mistaken for other conditions. Up until now, researchers have also been unable to find any underlying medical conditions that explain its onset. Characterized by extreme fatigue that lasts for six months or longer, CFS worsens with physical and mental activity but doesn’t improve with rest.
Chronic headaches, food intolerance, sore throat, enlargement of the lymph nodes, gastrointestinal problems, abnormal blood-pressure and heart-rate events, and hypersensitivity to light, noise or other sensations are the other hallmarks of this condition, say the researchers. An accurate estimation is difficult to determine for the one-to-four million range of Americans affected by the condition because the initial symptoms are often mistaken for conditions such as hypochondria.
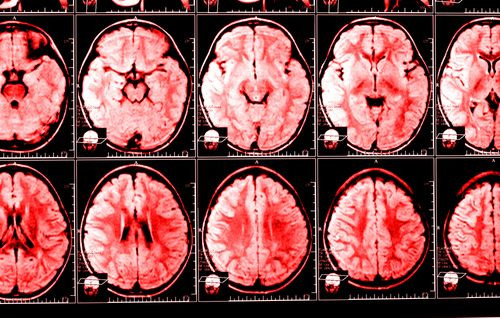
But the new study, published in Radiology, will help in more accurate diagnosis. "Using a trio of sophisticated imaging methodologies, we found that CFS patients' brains diverge from those of healthy subjects in at least three distinct ways," said coauthor Michael Zeineh.
Montoya, who has been tracking around 200 suspected patients for several years, says that CFS can affect a patient long-term, even as long as 30 years. This new diagnosis will not only provide a CFS-specific diagnostic biomarker, but may also help in “identifying the area or areas of the brain where the disease has hijacked the central nervous system," Montoya said.
The investigators compared brain images of 15 CFS patients with 14 healthy age-and sex-matched controls. The study found the following key differences.
- CFS patients had an overall reduction in brain white matter than healthy controls.
- CFS patients showed a consistent abnormality in the right arcuate fasciculus, a particular part of a nerve tract that connects the frontal lobe and temporal lobe.
- CFS patients had thickened gray matter at the two areas of the brain connected by the right arcuate fasciculus, compared to the controls.
While reduction in the white matter was expected, what surprised the researchers was the abnormality in the right arcuate fasciculus. A relatively unexplored region of the brain, the team found that there was a strong correlation between the degree of abnormality in a CFS patient's right arcuate fasciculus and the severity of the patient's condition, as assessed by performance on a standard psychometric test used to evaluate fatigue.
The findings are a huge step forward, but the researchers are quick to point that more extensive studies need to be conducted to corroborate these findings.
Source: Zeineh M, Montoya J, et al. Radiology. 2014.
Published by Medicaldaily.com



























