Drug-Resistant 'Superbugs' Threaten To Reverse Century Of Medical Progress

Threatening to jam a century of medical progress, drug-resistant superbugs may soon render routine operations and medical procedures dangerous and deadly.
Worse yet, some solutions to curbing the antibiotic overuse may hurt people in poor regions of the world most susceptible to bacterial infections, necessitating that global leaders heed the wizened environmental maxim to "think globally, but act locally," leading researchers say.
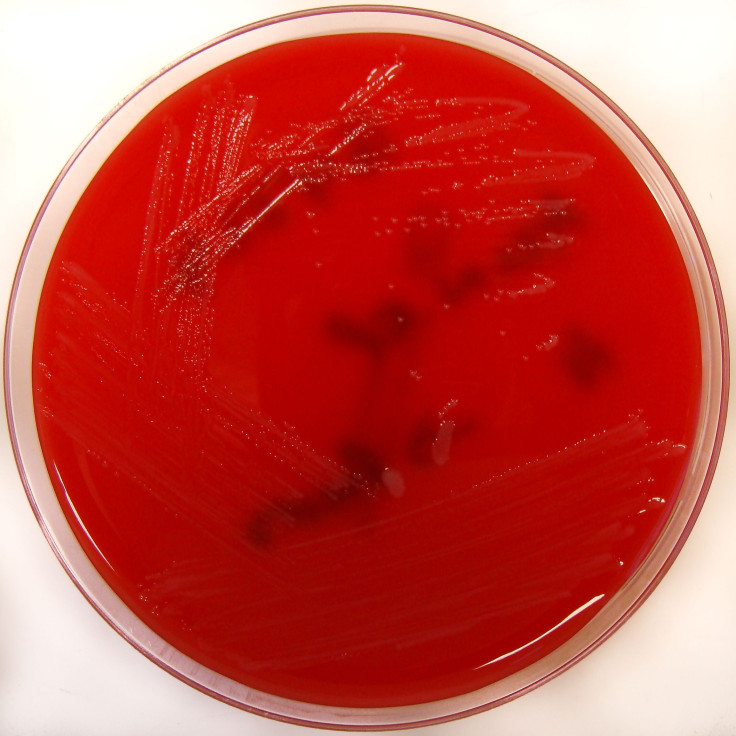
Marking the sixth European Antibiotics Resistance Day, the European Centre for Disease Control and Prevention (ECDC) warned of an increasing prevalence of infections resistant to carbapenem in hospitals throughout Europe. The drug is an important “last-line” antibiotic used to fight Acinetobacter infections spread in hospitals and healthcare settings, which may lead to deadly cases of pneumonia.
Data shows carbapenem-resistant infections increasing throughout Europe, especially in southern countries, said Marc Sprenger, director of the ECDC. “Since 2009, it has become increasingly common for hospitals to be faced with treating patients that have carbapenem-resistant infections, often meaning that old and toxic drugs are used,” he said.
The spread of Acinetobacter infections resistant to carbapenem rose to above 25 percent in eight of the 18 European countries reporting data to the ECDC, with Klebsiella pneumoniae bloodstream infections increasing by 5 percent in five countries between 2009 and 2012.
However, 17 of the 38 EU countries have thus far failed to develop guidance for hospitals to halt the spread of dangerous drug-resistant infections.
"There is an urgent need for all European countries to have in place national guidance documents, so that hospitals faced with carbapenem-resistant infections can take action to control the spread and minimise the impact of outbreaks on patients," Sprenger said. “Together with infection control measures, improving antibiotic use is the most important action needed to greatly slow the very worrying development and spread of antibiotic-resistant bacteria.”
In an report published in The Lancet, Otto Cars, a medical researcher at Uppsala University in Sweden, described an international investigation by “ReAct Action on Antibiotic Resistance, a collaboration of 26 leading experts in the field.
"The causes of antibiotic resistance are complex and include human behaviour at many levels of society; the consequences affect everybody in the world", he said in a statement. "Within just a few years, we might be faced with unimaginable setbacks, medically, socially, and economically, unless real and unprecedented global coordinated actions to improve surveillance and transform the way antibiotics are regulated and developed are taken immediately."
Among key problems, widespread overuse of antibiotics in medicine and agriculture has accelerated the evolution of drug-resistant bacteria, exacerbated by the slow development of new drugs by pharmaceutical companies.
"Only now has the awareness and urgency of the problem of antibiotic resistance reached a level that a new sustainable global system to counteract these problems can be built," Cars said. "Addressing these problems will require nothing less than a fundamental shift in how antibiotics are developed, financed, and prescribed."
Like so many other problems in the world, the threat of drug-resistant bacteria must be solved politically. Experts in agreement with Cars say international leaders must commit to investing in new ways to finance drug development, moving away from free market economics. Others solutions that merely curb the use of antibiotics would disproportionately affect people in poorer regions desperately dependent upon antibiotics for survival.
On a global level, drugs are developed with expectations of high sales volume, leading to aggressive marketing and salesmanship contributing to the very overuse helping to speed the evolution of superbugs. And on a microeconomic level, individual physicians chase financial incentives by prescribing more of these drugs, even when unneeded.
Thus, the entire profit-driven model of antibiotic drug development must be rejiggered, Cars and his colleagues conclude, before it’s too late.



























