Industrial Farm Workers Carry More Antibiotic-Resistant Staph Bacteria Than Organic Farmers
Antibiotic-resistant bacteria, particularly MRSA (methicillin-resistant Staphylococcus aureus), have emerged in increasing numbers over the past few years. First seen in European farm settings, they then moved to communities and hospitals. Scientists are now trying to find ways to prevent the same thing from happening in the U.S., where they are already found among farmers in livestock operations. According to a new study, the problem may lie in their noses.
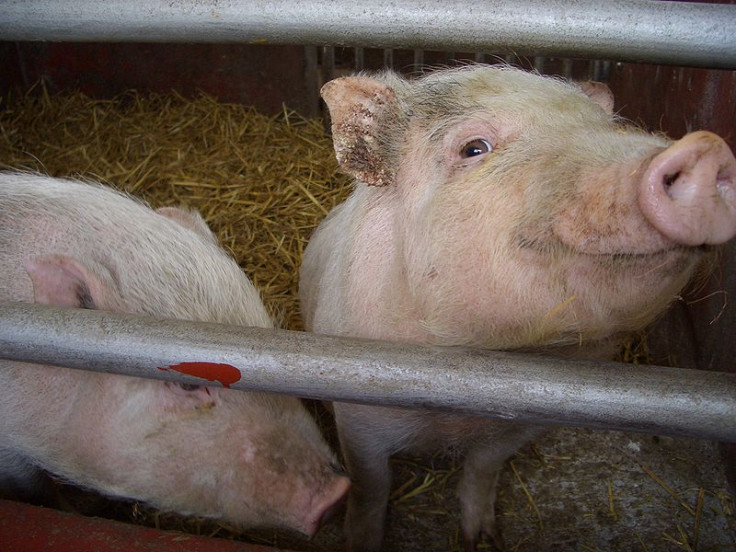
The industrial livestock industry is rife with antibiotics use. Animals are typically grown in large confinement buildings where antibiotics are loaded into the feed and water, however, its purpose isn't for fighting infection, but for promoting growth. As a result, Staph bacteria are able to become resistant to antibiotics over time because of their consistent exposure to such chemicals, the Smithsonian reported.
The study, conducted by researchers at Johns Hopkins Bloomberg School of Public Health and elsewhere, found that industrial livestock workers had much higher amounts of antibiotic-resistant Staph in their noses than workers at antibiotic-free farms--these farms typically raise their animals in pastures. They interviewed workers from both types of farms, and collected nose swabs, which were taken back to the lab. They tested the Staph in these swabs for resistance to antibiotics and genetic markers that indicated the bacteria came from livestock.
Overall, both groups had similar amounts of normal Staph — the kind that can be eliminated with antibiotics — but they found that multidrug-resistant Staph (MDRSA) was present in 37 percent of industrial farm workers, compared to only 19 percent of the workers at the antibiotics-free farms. Additionally, they found that 56 percent of the industrial farm workers had tetracycline-resistant Staph bacteria, compared to only three percent of those at antibiotics-free farms. Tetracycline is an antibiotic frequently prescribed for infections.
With strains of these bacteria already showing up in livestock workers in Iowa and North Carolina, scientists are concerned that the bacteria might spread in the same way it did in Europe. Iowa and North Carolina are already the first and second largest hog producers, respectively, in the United States,
Antibiotic-resistant Staph bacteria can cause a range of illnesses. They usually begin as small red bumps, and quickly turn into deep, painful abscesses. Some bacteria can even burrow deeper into the body, causing a person to be susceptible to infections on the surface as well as in the bones and organs. The Centers for Disease Control and Prevention (CDC) says that treating these illnesses becomes much harder when Staph bacteria becomes resistant to multiple drugs.
The study's researchers say that more research into how agricultural practices contribute to the growth of antibiotic-resistant bacteria is necessary. Their next research will focus on how workers' family members, and other people who come into contact with them, are affected.
Source: Rinsky J, Nadimpalli M, Wing S, et al. Livestock-Associated Methicillin and Multidrug Resistant Staphylococcus aureus Is Present among Industrial, Not Antibiotic-Free Livestock Operation Workers in North Carolina. PLOS One. 2013.
Published by Medicaldaily.com



























