A Lot Of Premenopausal Women Experiencing Some Degree of Pelvic Pain, Especially Those With Endometriosis
Pelvic pain may be a silent burden for a significant amount of premenopausal women, a study published today in Human Reproduction claims.
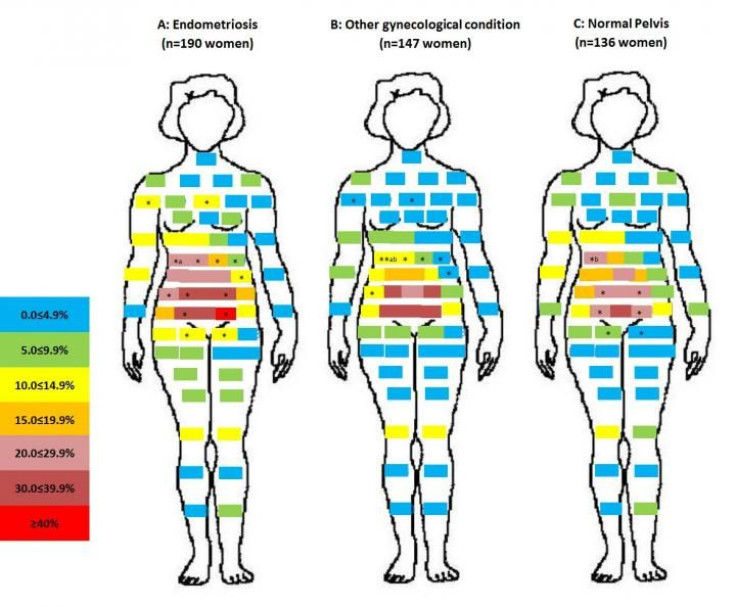
Researchers from the National Institutes of Health and the University of Utah School of Medicine interviewed more than 400 women between the ages of 18 to 44 who visited one of 14 different surgical centers about where and how often they experienced pain. Over 30 percent of those polled reported experiencing chronic, often cyclical, pelvic pain in the past six months.
And though two-thirds of these women were set to receive surgery because of a pre-existing gynecological condition, such as endometriosis, a relatively high percentage of those with no such condition reported chronic pelvic pain too — about 30 percent for the latter group.
"Our study suggests that many reproductive-age women are experiencing but not reporting some form of pelvic pain," said lead author Dr. Karen Schliep, a member of the Division of Intramural Population Health Research at NIH's Eunice Kennedy Shriver National Institute of Child Health and Human Development, in a statement. "If they aren't doing so already, gynecologists may want to ask their patients if they're experiencing pain, as well as the type and precise location of the pain, and offer treatment as appropriate. Similarly, women should let their doctors know if they're in pain."
Women suffering from endometriosis, a condition where the cells that line the uterus mistakenly end up in other parts of the body, often surrounding the ovaries or the pelvis, were the most likely to encounter chronic pelvic pain, at over 40 percent, and for that pain to be especially severe. They were more likely to report pain during sex or a bowel movement and experienced more menstrual cramps.
In endometriosis, the misplaced cells continue to respond to the same monthly cues that signal the uterine lining to build up and then break down. But because these cells are awkwardly positioned and unable to be flushed out of the body through menstruation, they can inadvertently cause their owner bouts of intense pain, scarring, and even infertility.
The women sought surgery to remove suspect lumps from their pelvis, undergo tubal sterilization, or because of their existing pain, infertility, or problems with maintaining a regular period. That distinction might dampen the ability to interpret this study in broader terms. Women who are already in need of extra gynecological care might be more likely to be suffering from pelvic pain than the general population.
Still, the study does highlight the need to better evaluate and communicate with any woman who walk into a gynecologist's office. And to reassure women that their pelvic pain isn’t something they need to shoulder alone.
Source: Schliep K, et al. Human Reproduction. 2015.



























