Mad Cow-Like Brain Illness Found In British Family: The Mystery Of Prions
A British family has been found to suffer from a deadly brain illness, similar to mad cow disease, which has already been passed down through several generations without external transmission, a new study reports.
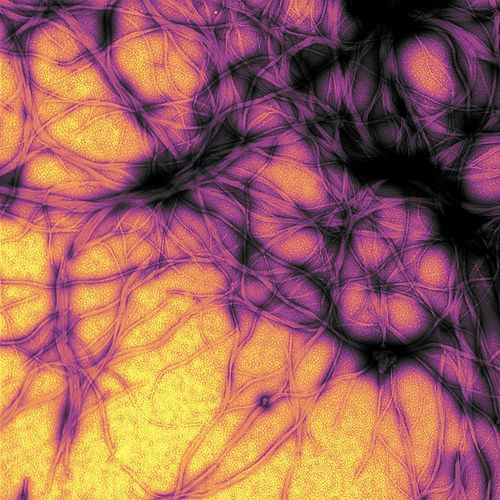
The family’s disease falls into the category of prion diseases. Prions aren’t bacteria, infections, fungi, or parasites; rather, they’re inert, like viruses, but attack the host’s brain via misfolded proteins, similar to the beta amyloid plaques of Alzheimer’s disease. Researchers involved with the current study believe better understanding prion diseases, and the way they penetrate brain tissue to cause damage, can open countless doors for further research into mental illness.
Led by prion expert Dr. Simon Mead, a neurologist and lead clinician at London's National Prion Clinic, the research team studied six of the 11 affected family members in detail, and five members through autopsy or biopsy samples. While the illness isn’t contagious like mad cow disease, the team found a given family member has a 50 percent chance of developing the disease at some point in his or her life. The disease is characterized by chronic diarrhea when patients were in their 30s, cognitive decline and seizures as they entered their 40s and 50s, and a risk of death before 60. Only one family member reached the age of 70.
"It has been passed on from generation to generation," Mead told HealthDay. Prion diseases, like many mental illnesses, currently have no cure or treatment. "But we are developing treatments, and hope to start clinical trials soon,” he added.
Other forms of prion disease include Fatal Familial Insomnia, a late-occurring disorder marked by intense and prolonged insomnia that leads to dementia, weight loss, and death — along with Creutzfeldt-Jakob disease, which scientists sometimes call the human version of mad cow disease because of how it pokes holes in the brain, creating a similar sponge-like texture.
However, prions aren’t totally antagonistic. A wealth of research into healthy prions, those being ones that are correctly folded, has found the proteins play an integral role in maintaining stable myelin sheaths that surround nerves. A 2010 study found four different strains of mice lacking the prion protein gene experienced myelin damage just six weeks after birth. By the two-month mark, the sheaths had grown increasingly demyelinated, making the mice extremely sensitive to pain.
"Because there is no myelin damage at birth, we assumed prions are needed to maintain the quality of the myelin sheath, which diminishes throughout life," noted study leader Dr. Adriano Aguzzi, of the University Hospital of Zurich, according to Nature. When Aguzzi and his team introduced prion proteins back into the nerves, demyelination ceased.
Unfortunately, the prion diseases suffered by the present family has no treatment or cure. Unless the family stops passing the disease through their blood line via reproduction, scientists believe it will continue manifesting in future generations.
What’s curious about their particular disease, Mead said, is how it attacks the intestines along with the brain. Normally, prion diseases remain localized in the host’s skull. "Most prion diseases cause damage in the nervous system," he said. "Prions are toxic to brain cells." As such, he and a team of researchers are working on a way to rejuvenate the body’s immune system to combat the intestine-targeting proteins, in addition to unearthing the links between prion diseases and Alzheimer’s, as they believe better understanding one may lead to uncovering insights into the other.



























