Mental Illness Found In Brain Folds Show Success In Judging Book By Its Cover
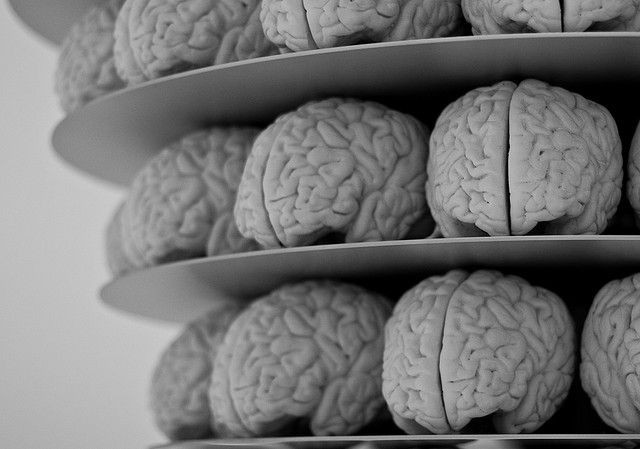
The hills and valleys of your brain should, more or less, look a certain way. Each intricate fold may be slightly different than those of the person’s next to you, but science is finding the healthy human brain doesn’t change much from head to head — just as a bicep may be a bit more bulging among bodybuilders but otherwise the same muscle.
The more 3D technology progresses, the more scientists are learning how to screen for abnormalities in these hills and valleys, formally known as gyri and sulci. They can take a picture of your brain, for instance, and render it on a computer to check for gaps where there should be gray matter. Or they can compare your brain to your relative’s brain, which is beginning to show early signs of deterioration, and make assessments on your risk.
In truth, it’s not so much the folds themselves that reveal brain health as much as what those folds say about the neurons, or brain cells, underneath. “The disturbances in connections between brain regions implicated by the changes in cortical folding could provide critical clues to deficits in the integrity of brain circuits,” said Dr. John Krystal, editor of the journal Biological Psychiatry, in a statement.
Most recently, scientists from Harvard University analyzed cortical folding for traces of schizophrenia, schizoaffective symptoms, and bipolar disorder. They used a measuring tool known as the gyrification index, which gives researchers a baseline count to refer to after they’ve produced a digital model of the brain. The more folds that are missing, or the lower the score on the index, the greater the likelihood certain functions are absent. From observation of 931 participants, made up of random subjects and one of their family members and healthy controls, scientists found cortical folds could indeed mark familial risk for psychotic illness.
"This study lays groundwork for further understanding of the causes of psychotic disorders,” commented senior author Dr. Matcheri Keshavan, a professor at Harvard Medical School.
Scientists are finding other outlets to check for gyrification. As the medical landscape stands now, doctors have few ways to reliably check how the treatment for psychotic illness is going. While some people may simply not respond to the prescribed treatment, others may show improvements outside the specified window of time, dating from their first psychotic episode.
A study in 2013 sought to ameliorate that issue. Researchers again took to studying gyrification defects, this time among patients who had been given 12-week antipsychotic treatment regimens. Specifically, they were looking for whether patients who didn’t respond to this treatment had already begun the regimen with cortical defects. Ultimately, they found the worse patients responded to treatment, the more severe their hypogyria — the absence of cortical folds.
“Gyrification appears to be a useful predictor of antipsychotic treatment response,” the team wrote in the abstract of their report. “Early neurodevelopmental aberrations may predict unfavorable prognosis in psychosis, irrespective of the existing diagnostic boundaries.”
There is also some research to suggest schizophrenia patients aren’t alone in experiencing fold loss. Alzheimer’s disease sufferers have been found to experience the same condition: As the brain’s supply of amyloid plaque builds, once healthy tissue falls to clouding and the eventual destruction. And by the same logic, more folds generally predict greater memory and intelligence. One way to accomplish this, especially for people with a family history of illness, is to meditate.
A 2012 study confirmed it: "The positive correlation between gyrification and the number of practice years supports the idea that meditation enhances regional gyrification,” said neuroimaging researcher and assistant professor at UCLA, Eileen Luders. So start practicing your Oms and keep your brain folded, as it should be.
Published by Medicaldaily.com



























