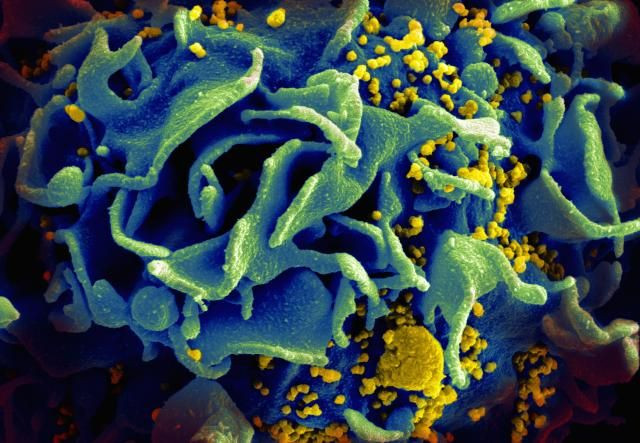
A New HIV Treatment? Antibody Infusion Supresses The Virus In Real-Life Patients
It’s no cure, but it might someday lend much needed support in our war against HIV.
Earlier this December in Science Translational Medicine, a large collaboration of researchers published their latest findings on a potential treatment for the virus: the infusion of a specific antibody designed to fight back against a wide array of HIV strains at the same time (a technique known as passive immunization). In a preliminary trial of 23 patients, the researchers found that the antibody, called VRC01, could safely and noticeably lower the level of HIV in a chronically infected person’s blood, though only if that person wasn’t already on antiretroviral therapy (ART).
“Passive immunization with neutralizing antibodies could therefore aid in viral suppression in HIV-infected individuals,” the authors concluded.
First considered for clinical development in 2010, VRC01 is part of a class known as broadly neutralizing antibodies (bNAbs). While most neutralizing antibodies are specifically tuned to combat a single strain of a single infectious pathogen (or other foreign invader), VRC01 and its ilk are capable of responding to multiple versions of the same virus (other antibodies simply bind to a foreign invader, so that the rest of the immune system can destroy it). That ability has tantalized researchers about their potential in fighting back against viral diseases that rapidly mutate as a means of protection, such as influenza and HIV. These bNAbs, though they can now be cloned in the lab, are first cultivated from the blood of individuals who have lived with HIV for at least several years.
Funded by the National Institutes of Health (NIH), this latest study, a Phase 1 trial intended mostly to prove safety, gave infusions of VRC01 to 15 volunteers already on ART and eight volunteers who were untreated otherwise. The ART group was given two doses, 28 days apart, while the untreated group only received one.
There was no recognizable drop in the amount of HIV left lurking behind in those taking ART. In six of the eight untreated volunteers, however, there was a sharp decline — more than 10-fold — of HIV. Two of these volunteers responded especially well, with VRC01 suppressing their HIV to undetectable levels for over 20 days before the VRC01 wore off. The two untreated who showed the least response appeared to have HIV strains already resistant to VCR01, while the two best-performing appeared to have the lowest viral loads and susceptible strains. Also importantly, none of the volunteers had particularly adverse side effects.
Though encouraging, these findings come with obvious caveats. For one, even should VRC01 continue to be effective, it’s hard to envision it as a functional cure, given that a therapeutic dose only lasts for a period of weeks at best. Second is the exorbitant price, with antibody therapy likely costing thousands per session. Third, as shown here, certain HIV strains already carry a degree of resistance against VRC01. The HIV found in the remaining four untreated volunteers who were given VRC01 appeared to be developing resistant strains as the trial progressed as well.
Acknowledging these considerations, the researchers believe VRC01’s likely future is to be used as another method to maintain viral suppression in combination with present or future treatments, much like how ART currently works. Pilot studies of other bNAbs in HIV-infected subjects published recently have produced similarly encouraging, if cautious, findings.
If we’re shooting for the sky, though, the primary advantage that VRC01 and other bNAbs may have over ART is in their potential application as part of an effective vaccine someday.
Source: Lynch R, Boritz E, Coates E, et al.Virologic effects of broadly neutralizing antibody VRC01 administration during chronic HIV-1 infection. Science Translational Medicine. 2015.



























