Pres. Obama's Precision Medicine Initiative, The Human Genome Project, And Your Individualized Genetic Data
Inside every human being is 23 chromosomes, housing three billion pieces of genetic information that contains the color of our eyes, the curve of our nose and our lifelong susceptibility to disease. Medicine has known for decades this is where the instructions for life reside. All they needed to do was learn how to decipher the complex human blueprint.
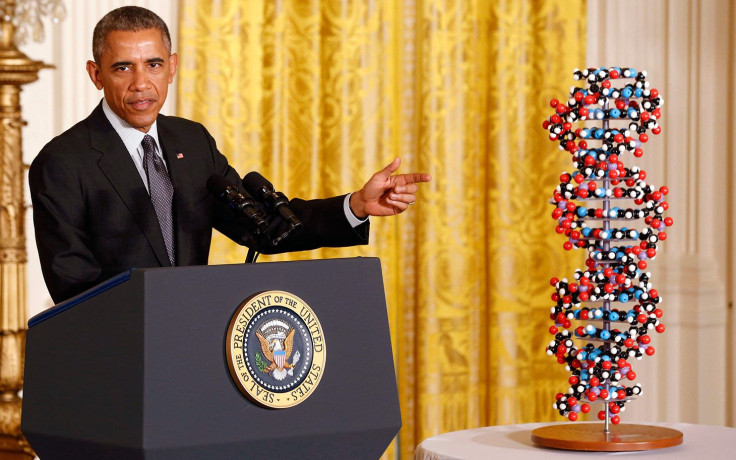
When President Obama announced in his State of the Union Address on Jan. 20, 2015 that the White House, through the National Institutes of Health, would allocate a $215 million investment into a Precision Medicine Initiative, Mayo Clinic rejoiced. Mayo’s Center For Individual Medicine practices under the term “individualized medicine,” but whether it’s referred to as “personalized,” “precision,” or “individualized,” the future of medicine is clearly moving toward one goal: tailoring the prevention, diagnosis, and treatment of disease to specific patients through the use of the most advanced technologies available.
The new funding will provide a portion of the means necessary to accelerate biomedical discoveries by collecting the genetic data for one million Americans. The hope is that, with that information, researchers can discover genetic causes of disease and to match the precise drug treatment designed for your DNA — instead of forcing one-size-fits-all procedures.
“You can match a blood transfusion to a blood type,” Obama said. “What if matching a cancer cure to our genetic code was just as easy? Just as standard? That’s the promise of precision medicine, delivering the right treatments at the right time, every time, to the right person.”
From Promise To Practice
“Don’t tell me how you’re going to treat kidney cancer. Tell me how you’re going to treat my kidney cancer,” said Dr. Alexander Parker, the associate director for Mayo Clinic’s Center for Individualized Medicine. “That’s what we all want—individualized answers to our questions. On the other side, that’s what physicians have always wanted to do, too. They want to get answers tailored specific to the patient sitting in front of them.”
This is not a new concept. Six thousand years ago, Hippocrates, the father of medicine, stated: “It’s far more important to know what person the disease has than what disease the person has.”
By engineering the technology and implementing a system for routinely sequencing genomes, scientists will, in theory, unearth the information that will empower patients to play a much more proactive role in driving their health outcomes than ever before. But in practice, there’s still a lot of work to do.
The Human Genome Project and its ambitious goals were first articulated by the U.S. National Academy of Sciences in 1988. Fifteen years later, when the first human genome was sequenced and published in the journal Nature, it was simply an achievement of having all of the human genetic code’s three billion base pairs sequenced and mapped out. Next came the challenge of reading the enormity of it, one page at a time. That same year, The Human Genome Research Institute, a branch of the National Institutes of Health, announced to the public what the next 50 years of medical discovery should look like:
The challenge to researchers and scientists now is to determine how to read the contents of all these pages and then understand how the parts work together and to discover the genetic basis for health and the pathology of human disease. In this respect, genome-based research will eventually enable medical science to develop highly effective diagnostic tools to better understand the health needs of people based on their individual genetic make-ups, and to design new and highly effective treatments for disease. Individualized analysis based on each person's genome will lead to a very powerful form of preventive medicine.
The Price Tag for Precision
The problem, though, has been affording to sequence mass quantities and apply practice to the entire spectrum of health care. Sophisticated methods of genomic sequencing and analysis have created innovative opportunities to further tailor care for each patient, but in order to decide on a direction of treatment or to assist on a diagnosis, researchers need large sample sizes of patients. Without large groups, studies become limited and stunted in their potential. So, while individual genome sequencing is a critical step, it is sequenced populations that will provide clinical tools to better understand the complex mechanisms underlying a patient’s disease and condition, and to better predict treatment outcomes.
It is because of this that Obama’s investment in the Precision Medicine Initiative was not just a financial contribution. Out of the $215 million set aside in the president’s 2016 Budget, $130 million will go to the National Institutes of Health for developing a voluntary national research cohort of a million or more patients. With such a large population, it will lay the foundation for genomic sequencing on a scale unlike anything researchers have done before. It will also propel forward a new way of performing research by engaging and interacting with participants through a data-sharing network, in which genomes will be analyzed and compared.
“We’ve had a love-hate relationship with this because we have never been able to look at the entirety of our DNA,” Parker said. “We’ve always had to look at little, tiny pieces at a time.” Parker has been working on genome sequencing since 1996. Back then, he says, the frustration was that they would have to commit tons of time and resources to looking at tiny regions with no guarantee of success. “And spending months focusing on that little area, only to find out that that’s not where the answer was — incredibly, incredibly frustrating.”
It took 15 years to sequence the first genome, and the project cost a staggering $3 billion. And then, after that, it took eight years to bring the cost of sequencing one genome down to $10 million — a price tag that could revolutionize health care, but only for for someone like Bill Gates or Mark Zuckerberg.
But the technology has advanced so rapidly that within 12 years it has gone from taking months to complete at $100,000 per person to about $1,000 per person, their results coming in within 24 hours. That’s within reach for most Americans, and makes sequencing a force to be reckoned with in medicine. That very reasonable price tag is also what’s driving every academic institution with an individualized medicine research center to race to implement an adequate system to collect, organize, and analyze the genomic data.
“What we needed, what we always wanted, was the equivalent of a GPS,” Parker said, “where all roads and everything was known and we could look at the entirety of it all at once and find answers instead of trying to guess where to look. The reason why we’re here is we got our GPS when we cracked the code and sequenced the first human genome. The wait is over. Medicine is changing and transforming. We have moved from promise to practice.”
Published by Medicaldaily.com



























