The Promise of Immunotherapy In The Fight Against Cancer
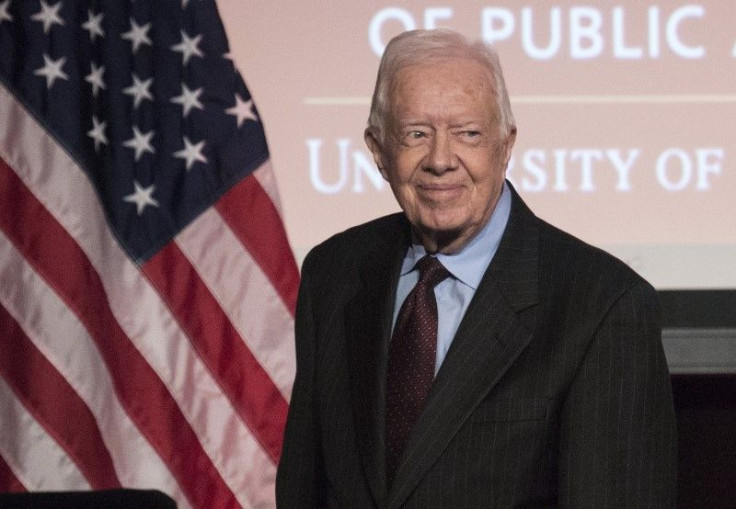
Early December’s announcement by former President Jimmy Carter that his cancer had vanished from MRI scans galvanized the general public and drew everyone's attention to the progress scientists have made in manipulating the immune system to treat cancer. Revealing his progress to the nation by way of a group of children illustrates the optimism that is spreading among scientists and clinicians in the field.
Mr. Carter suffers from metastatic melanoma, and cases like his — where lesions have spread to the brain and liver — are particularly difficult to treat. The overall five-year survival rate for the disease hovers around 16 percent. The former president and many others credit a novel immunotherapy drug, which he received in addition to surgery and radiation therapy, for his astounding remission.
The idea to mobilize the immune system to fight cancer has been around for decades but until recently its proponents were considered overly optimistic, if not outright misguided. After all, the immune system is a complex, tightly orchestrated system and it seemed clinically implausible to find a way to control the body’s own defenses to attack its “abnormal self” in safe and predictable ways.
But the painstaking fundamental research that is revealing how the immune system works is starting to pay dividends in clinical practice: Hardly a week goes by without a report of a new milestone as immunologists refine immunotherapy-based strategies as a powerful weapon in the arsenal against cancer.
Conventional therapies such as radiation, some chemotherapies and cytotoxic anti-cancer drugs kill tumor cells directly. Immunotherapies, by contrast, leverage a different but no less potent mechanism of killing tumor cells. Instead of targeting the tumor itself, they rally a patient’s dormant immune cells to do the job. Prominent among them are T cells, the immune system’s “warrior cells,” which normally attack foreign cells or cells harboring bacteria or viruses.
Scientists initially found that T-cell responses to tumor cells were unusually sluggish. In the last decade they discovered why: Molecular signals emitted from a tumor, or other cells caught up in the tumor environment, undercut the beneficial response to attack, making tumor cells effectively invisible to the immune system.
Pembrolizumab, the drug Carter received, yanks the virtual immunological cloak of invisibility from tumor cells, allowing T cells to home in on cancer cells and destroy them. The drug is an example of a new class of cancer drugs known as checkpoint blockade inhibitors. They neutralize inhibitory switches that are hardwired into T cells, usually a helpful way to prevent our immune system from turning against our own cells. Pembrolizumab was fast-tracked for FDA approval last year after producing startling and long-lasting results in the treatment of metastatic melanoma and certain types of lung cancer.
Other groups have set their sights on specially engineered T cells called chimeric antigen receptor T cells (CARTs), to direct immune system cells to cancer cells that display telltale surface markers. As part of the treatment, T cells are removed from a patient’s immune system and modified so they can identify tumor cells as foreign. When reintroduced to the patient, these engineered cells seek and destroy the targeted cells. Although still in the early stages of clinical development, they have shown promise in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia and acute lymphocytic leukemia.
Another approach, known as adoptive immunotherapy, faces one of the biggest challenges of cancer immunotherapy head on: Unlike viruses and bacteria that invade the body from the outside, tumor cells often look too much like normal cells for the immune system to recognize them as foreign. Adoptive immunotherapy exploits the fact that cancer cells accumulate a collection of mutations as they travel down the path of malignant transformation. Some of these changes may be fueling cancer cells’ uncontrolled growth or they may be innocent bystander mutations. But both types of genetic aberrations can result in what are known as “tumor-specific“ or “neoantigens.” These are ideal targets for scientists to train the immune system to distinguish heavily mutated cancer cells from their normal counterparts. Since mutation is the basis of cancer, few types of cancer may escape from this logical, measurable, and therefore rational approach.
First, a sample is taken from a patient’s tumor and its DNA is sequenced to identify tumor-specific mutations. They are then tested against a patients’ own T cells to identify which ones are recognized. These tumor-specific antigens can then be used to expand a patient’s tumor-specific T cells into a highly focused army of killer cells or can form the basis of a highly personalized cancer vaccine. If the process successfully duplicates what has already been shown in mice, cancer immunotherapy that has been custom-tailored to a patient’s tumor will not only fight the primary tumor but will continue to hunt down stray cancer cells before new metastases can establish themselves. This approach puts the “personal” into personalized medicine and has only become possible thanks to dramatic advances in technology and decades of intensive research into the most fundamental mechanisms governing the immune system.
Cancer researchers generally agree that there need not be a single way to eradicate all tumors. Instead, the current consensus is that effective approaches will be multi-pronged and patient-specific, integrating surgery or radiation when appropriate with oncogene-targeting chemotherapies and powerful new interventions that put teeth in a patient’s immune response. With effective immunotherapies, more than ever before, the treatment of cancer will become rational, highly effective, and much less injurious to those we treat.
Dr. Steve Wilson is the executive vice president and chief operating officer of the La Jolla Institute for Allergy and Immunology, one of the top five research institutes in the world solely focused on the immune system. He's also the co-prinicpal investigator and project director of the NIH's Immune Epitope Database and Analysis Resource, and exective director of the Institute's Functional Genomics Center. Prior to his current position, he was a research fellow of both the NIH and the National Multiple Sclerosis Society, where he published research on the immunological basis of autoimmune disease. Wilson holds a BSA in Microbiology and a PhD in Immunology from the University of Arizona's School of Medicine.



























