PSA Test For Prostate Cancer Could Be Revolutionized With New, Painless Imaging Technique

The same techniques used to produce images of prenatal ultrasound scans can be used to highlight problematic tumor tissues in prostate exams, new international research finds.
Each year, nearly 20 million American men undergo the potentially unnecessary experience of a prostate-specific antigen (PSA) test. Designed to screen for the possible trace of cancer, the test relies on collecting blood samples to determine how high or low a man's antigen levels are. If the levels are too high, doctors will then draw just over a dozen, often painful, biopsies from the patient’s prostate. The problem with the PSA test is its high sensitivity but low specificity — meaning that it detects cancer very easily, but can’t rule out cancer without taking numerous samples.
The test also isn’t fool-proof. In 2012, the United States Preventive Services Task Force issued a set of guidelines on PSA tests, maintaining that false-positive tests were associated with fever, infection, bleeding, and pain. Men may also become impotent and suffer from urinary incontinence as a result of the test, the USPSTF asserts.
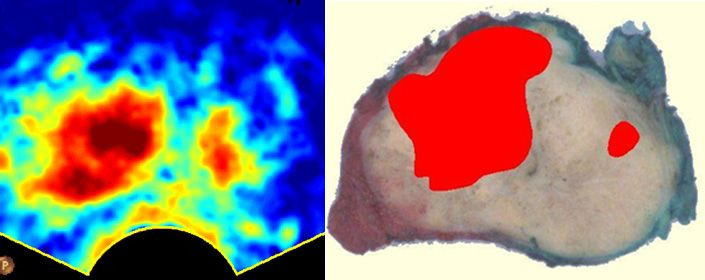
In their latest research, scientists from Eindhoven University of Technology sought to improve upon this test with potentially no biopsies required. The new technique, developed by team leader Massimo Mischi, relies on the way cancer cells grow within the prostate. When cancerous tissue grows, it produces large numbers of small blood vessels that proliferate according to a very specific pattern. When patients are injected with a contrasting agent, the patterns become visible, and an advanced computer can reveal where the cancer is. The entire process takes approximately a minute.
“Because of the poor screening by the blood test about 75 percent of patients undergoing biopsies in retrospect did not need these biopsies,” Mischi, who will be presenting his team’s findings on April 14 at the European Association of Urologists Congress in Stockholm, recently explained. The biopsies turned out to be unnecessary, he says, “because cancer was not present.”
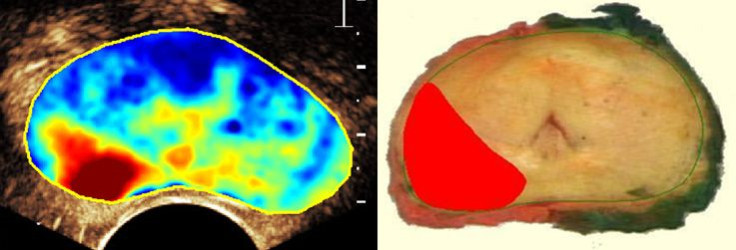
His new method not only reduces the amount of money wasted on these negative biopsies, but also makes the process more tolerable. For the remaining portion of men in whom the imaging technique does find cancer, taking biopsies will still be easier because the exact location of the tumor is clear. Their study compared 24 images of prostates visualized using the new technique with the actual gland removed by operation. By and large, the images offered a consistent picture of the tumor’s size and location.
Upcoming for Mischi and his colleagues is a comparative study of the two methods in two Dutch hospitals and the Academic Medical Center Amsterdam. At least 250 men will participate in the study, which, if proven successful, will carry into surrounding hospitals. Mischi argues the implementation process will be, like the test itself, short and painless, as the existing ultrasound scanners can pull double duty.
As the leading cause of cancer-related death in men, prostate cancer screenings stand much to gain from improved accuracy and reduced invasiveness. What’s more, the screening technique isn’t limited to just men. “What we can do is translate this type of research toward other types of cancers that also need advanced diagnostic systems,” Mischi said, “like for instance, breast cancer, which has the same incidence and the numbers of prostate cancer for women.”
TU/e BIG nominees: Massimo Mischi from IPSOvideo on Vimeo.
This story has been corrected to reflect that PSA tests are minor blood tests, which may precede invasive biopsies, and are not biopsies themselves.



























