Scientists Engineer Stem Cells That Can Identify and Destroy HIV Inside Living Mice
Genetically engineered human stem cells have been shown to be capable of suppressing HIV by virus-infected cells in living mice, according to scientists who hope that the recent breakthrough will lead to a cure for HIV patients.
Previous HIV research largely focused on vaccines or drugs that aim to slow the virus’s progression, but the latest findings offers hope of a potential treatment that can completely eradicate HIV from an infected patient, according to researchers from the latest study published April 12 in the journal PLoS Pathogens.
"We believe that this study lays the groundwork for the potential use of this type of an approach in combating HIV infection in infected individuals, in hopes of eradicating the virus from the body," lead researcher Scott G. Kitchen, an assistant professor of medicine in the division of hematology and oncology at the David Geffen School of Medicine at University of California, Los Angeles said in a statement.
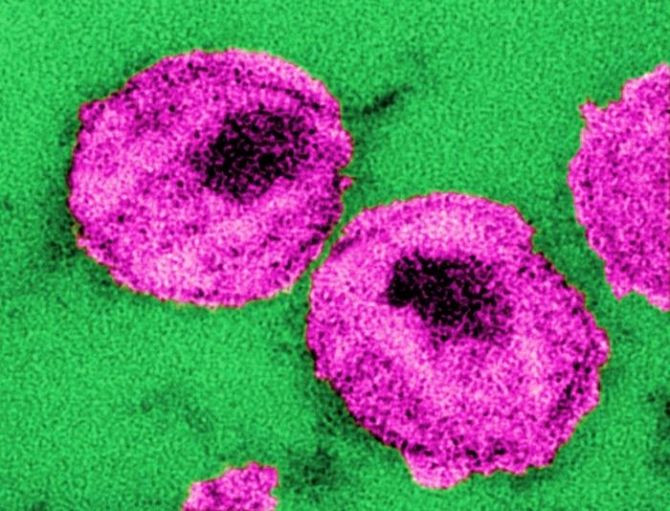
Previously, scientists took CD8 cytotoxic T lymphocytes or "killer" T cells that fight infections from HIV patients and identified the molecule that guides the T cells in recognizing and killing HIV-infected cells.
While these HIV-destroying cells exist in the body, they are not in great enough quantities to eradicate the virus from the body, according to researchers.
After identifying the molecule, researchers cloned the receptor and used it to genetically engineer human blood stem cells that were placed into human thymus tissue that had been implanted in mice, which allowed them to observe the reaction in a living animal model.
Past findings show that the engineered stem cells developed into a large population of mature, multi-functional HIV-specific CD8 cells that could specifically attack cells containing HIV proteins.
However, researcher noted that HIV-specific T cell receptors need to be matched to an individual which is similar to how an organ is matched to a transplant patient.
Researchers from the current study replicated previously engineered human blood stem cells and placed them in a surrogate mouse model, in which HIV infection resembles the disease and progression in humans.
Afterwards, researchers conducted a series of tests on the mice’s peripheral blood, plasma and organs two weeks and six weeks after introducing the genetically engineered cells and discovered that the previously depleting number of CD4 "helper" T cells, white blood cells that help fight off infections, actually increased and levels of HIV in the blood decreased.
While the latest research has for the first time provided evidence that engineered cells were capable of developing and migrating to the organs to fight infection there, researchers noted that because human immune cells reconstruct at a lower level in genetically engineered “humanized” mice, which had immune systems that were mostly reconstructed, than they would in humans, the virus may mutate slower in mice than in human hosts.
They suggest that a potential way to address this limitation would be to use multiple engineered T cell receptors to adjust for the higher potential for HIV mutation in humans.
"We believe that this is the first step in developing a more aggressive approach in correcting the defects in the human T cell responses that allow HIV to persist in infected people," Kitchen said.
Researchers are currently working on developing T cell receptors that can be used in more genetically matched individuals and that will be capable of targeting different parts of the virus.



























