Treating PTSD With Psychedelics: How Ecstasy, The ‘Rave’ Drug, May Help Trauma Patients Overcome Painful Memories
Ecstasy may conjure images of shuddering dancers, bursting with energy at warehouse parties and raves. But scientists have for a while wondered about tapping into ecstasy’s hidden medicinal secret: a potential to be therapeutic for people with mental health issues, especially post-traumatic stress disorder (PTSD).
A new study out of the Imperial College London in England examined the psychedelic drug’s effect on certain parts of the brain, including areas that are linked to memory and emotion, and found that MDMA (methylenedioxymethamphetamine) could have a positive effect on anxiety as well as PTSD. “In healthy volunteers, MDMA seems to lessen the impact of painful memories,” Dr. Robin Carhart-Harris, an author of the study and a professor in the department of medicine at Imperial College London, said in a press release. “This fits with the idea that it could help patients with PTSD revisit their traumatic experiences in psychotherapy without being overwhelmed by negative emotions, but we need to do studies in PTSD patients to see if the drug affects them in the same way.”
The authors of the study analyzed twenty-five volunteers who experienced brain scans on two separate occasions — once after taking the drug, and once after taking a placebo, without knowing which they had been given. The study discovered that MDMA diminished activity in an area in the brain linked to emotions, called the limbic system, and also reduced communication between the medial temporal lobe and medial prefrontal cortex, which is associated with emotional control. This decrease in communication and activity in the limbic system was the “opposite” to what was seen in anxiety patients, according to the study’s press release.
“We found that MDMA caused reduced blood flow in regions of the brain linked to emotion and memory,” Carhart-Harris said in the press release. “These effects may be related to the feelings of euphoria that people experience on the drug.”
MDMA-Assisted Psychotherapy
This is not the first study to look into ecstasy’s effect on PTSD patients. Last year, researchers in Vancouver studied how the drug could be helpful in medicinal portions. Dr. Andrew Feldmer, a psychologist in Vancouver who helped run the study, notes that the amount of the drug ingested plays a large role in deciding whether or not it has the potential to be therapeutic. “The very same substance can be poison or medicine, depending on the dosage, depending on the circumstances in which it is ingested,” he said.
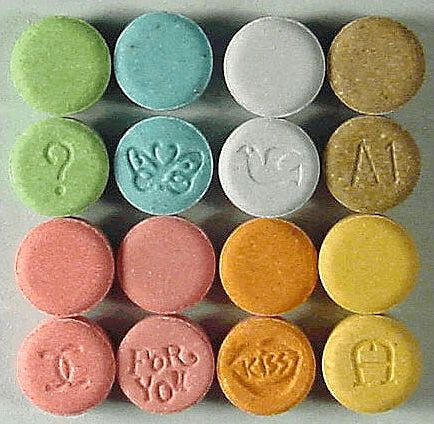
Organizations such as the Multidisciplinary Association for Psychedelic Studies (MAPS) have poured time and funds into researching medicinal benefits of psychedelic drugs like MDMA, as well as marijuana. On its website, MAPS explains that MDMA used for therapeutic purposes is not the same as the ecstasy sold on the streets. “Substances sold on the street under the name Ecstasy do often contain MDMA, but frequently also contain harmful adulterants,” MAPS writes. “In laboratory studies, pure MDMA — but not Ecstasy — has been proven sufficiently safe for human consumption when taken a limited number of times in moderate doses.” MAPS is planning on undertaking an eight-year, $18.5 million plan to help make MDMA an FDA-approved prescription medication.
In the meantime, the authors of the Imperial College London study have admitted they will need to do further research on the topic, and to next test actual PTSD patients for more clarified results. “The findings suggest possible clinical uses of MDMA in treating anxiety and PTSD, but we need to be careful about drawing too many conclusions from a study in healthy volunteers,” David Nutt, a co-author and professor of neuropsychopharmacology at Imerial College London, said in the press release. “We would have to do studies in patients to see if we find the same effects.”
Source: Carhart-Harris R, Murphy K, Leech R, Erritzoe D, Wall M, Ferguson B, et al. "The Effects of Acutely Administred 3,4- Methylenedioxymethamphetamine on Spontaneous Brain Function in Healthy Volunteers Measured with Arterial Spin Labelling and Blood Oxygen Level-Depending Resting-State Functional Connectivity." Journal of Psychiatric Neuroscience and Therapeutics. 2014.
Published by Medicaldaily.com



























