Alzheimer's Disease Patients With More Tau Protein In The Brain Face Greater Risk Of Cognitive Decline
Alzheimer’s disease, despite so many 21st Century medical advancements, remains a public health menace. The neurodegenerative disorder is progressive and incurable, with treatments merely slowing the progression of symptoms at best. A thorough understanding of what causes Alzheimer’s is necessary to find effective treatments, and for what it's worth, researchers have learned to associate certain phenomena with the condition, including a buildup of plaque and dysfunctional proteins in the brain.
A new study from the Washington University School of Medicine in St. Louis, however, suggests existing disease markers may have been partially misdirected. Most Alzheimer’s studies focus on an accumulation of the protein amyloid beta, the study authors said, while their findings point to another protein, tau, as potential early sign of mild cognitive impairment — a risk factor for Alzheimer's and dementia.
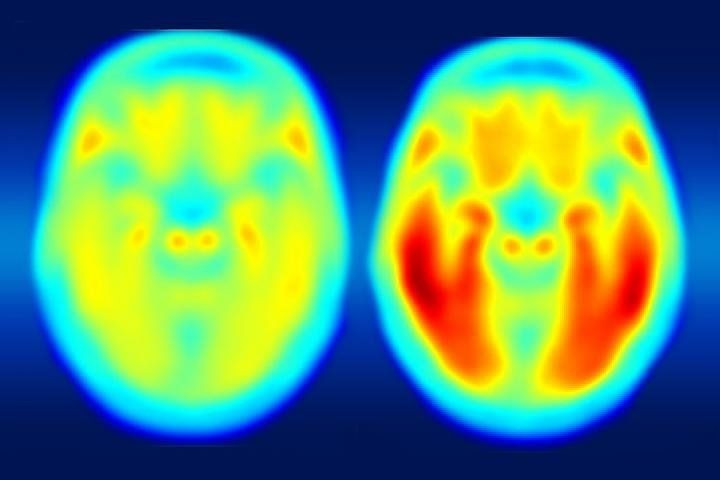
The imaging technology available to measure tau is fairly new, but the authors were able to use an imaging agent that binds to the protein in order to makes it appear on a positron emission tomography (PET) scan. After they compared images of patients with mild Alzheimer’s to those who were cognitively normal, they found that the tau protein was a more accurate predictor of dementia than the amyloid beta protein.
“Our work and that of others has shown that elevated levels of amyloid beta are the earliest markers of developing Alzheimer’s disease,” said Dr. Beau M. Ances, senior author of the study and associate professor of neurology at Washington University, in a statement. “But in the earliest stages of Alzheimer’s disease, even with amyloid buildup, many patients are cognitively normal, meaning their memory and thought processes are still intact. What we suspect is that amyloid changes first and then tau, and it’s the combination of both that tips the patient from being asymptomatic to showing mild cognitive impairment.”
A larger follow-up study is needed, but as is, these findings help establish tau as an important factor for other researchers to consider when tracking Alzheimer’s development and progression. Ances explained that this knowledge could help catch Alzheimer’s in its earliest stages.
“Usually we can only diagnose patients later in the disease process, when brain function already is diminished,” he said. “We want to develop ways to make an earlier diagnosis and then design trials to test drugs against amyloid buildup and against tau buildup.”
Ances said that while a cure is still a long way off, even a delay of symptom onset could make a huge different to patients, caregivers, and families across the globe. In addition to advancing treatment efforts, the study will also provide researchers with an additional tool to gather spatial information about Alzheimer's, where in the brain the condition manifests.
“Our new study suggests you can tolerate a certain amount of tau clumped in the hippocampus, but once it starts spreading to other areas, especially the lateral temporal and parietal lobes, that seems to be the tipping point,” Ances explained.
The imaging system capable of picking out tau has been approved for use in the context of clinical research trials, and may prove useful for imaging other types of brain disorders in addition to Alzheimer’s.
Source: Brier M, Gordon B, Friedrichsen K, McCarthy J, Stern A, Christensen J, et al. Tau and Ab Imaging CsF Measures, and Cognition in Alzheimer’s Disease. Science Translational Medicine. 2016.



























