For Cancer Screenings, When Do The Benefits Outweigh The Risks?
Cancer screening guidelines don’t always help patients understand the risks and benefits of the procedures, according to a new study. While it may seem like everyone should get screened for cancer, in many cases, screening can be unnecessary and even harmful to a patient — a double-edged sword.
In the study, researchers from the University of Michigan Health System examined 55 professional guideline recommendations for cancer screening, and they found that a large amount of them — 69 percent — didn’t fully explain the costs and benefits of the procedure. Cancer screening may find potential cancers sooner that can be treated early, but the risks of screenings can include false positives, overtreatment, and unnecessary, invasive procedures.
One 2015 study found that overdiagnosis is a common effect of increased screening, especially for thyroid cancers. Screenings have become much more developed and fine-tuned in recent years, giving them the ability to identify any type of tumor — even if they’re tiny, benign, and not life-threatening. Regardless, spotting any tumor calls for a doctor to act upon it, even if it’s better off untreated. This leads to an increase in diagnoses, costly treatments, and unnecessary procedures. On top of all that, a recent study published this year found that researchers are still uncertain as to whether cancer screening truly saves lives.
The University of Michigan researchers wanted to see how aware patients were of both the positives and negatives of cancer screening, as many people are often eager to get thoroughly screened without paying heed to the costs. They examined screening guidelines for breast, prostate, colon, and cervical cancers, among others — guidelines that had been issued by authoritative organizations, including the U.S. Preventive Services Task Force and the American Cancer Society. Only 31 percent of the guidelines reviewed explained both the benefits and costs of screening, while 55 percent were uneven in their explanations.
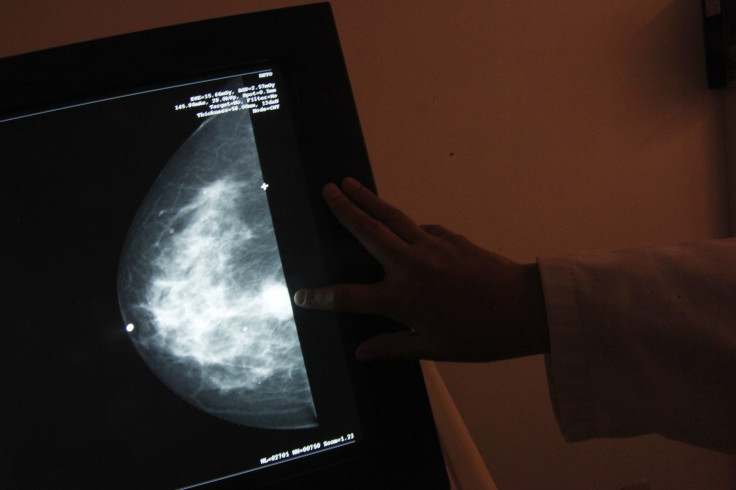
When it comes to breast cancer screenings, research has shown that their benefits outweigh the risks; the screenings have reduced the number of deaths from breast cancer. But each type of cancer is different, and each patient has a right to learn the costs and benefits of each screening.
“Almost all medical interventions have tradeoffs between different types of benefits and harms,” Dr. Tanner Caverly, clinical lecturer of internal medicine at the University of Michigan Medical School and an author of the study, said in the press release. “Patients rely on doctors to base screening recommendations on sound judgment as to whether, in their individual context, the benefits outweigh the harms. For this judgment, doctors need a clear understanding, in quantitative and comparable terms, about the degree of potential benefit and the degree of potential harm.”
Source: Caverly T, et al. Journal of the National Cancer Institute, 2016.



























