Immunotherapy Is The Future Of Cancer Research: 70% Of Multiple Myeloma Patients Find Recovery With New Treatment
Immunotherapy, or the use of a person’s own immune system to treat an infection or disease, has recently been at the forefront of cancer research. In a new study, researchers found that a form of immunotherapy could produce a “significant clinical response” in 70 percent of patients with a particularly deadly type of cancer known as multiple myeloma. These results not only highlight the potential of this exciting new field but also the importance of further immunotherapy research.
The study, published online in Nature Medicine, was conducted by researchers from the University of Maryland Medical Center. Twenty patients with an advanced form of multiple myeloma, a cancer of the plasma cells, underwent a stem cell transplantation of their own stem cells before being injected with around 2.4 billion genetically altered immune system T cells.
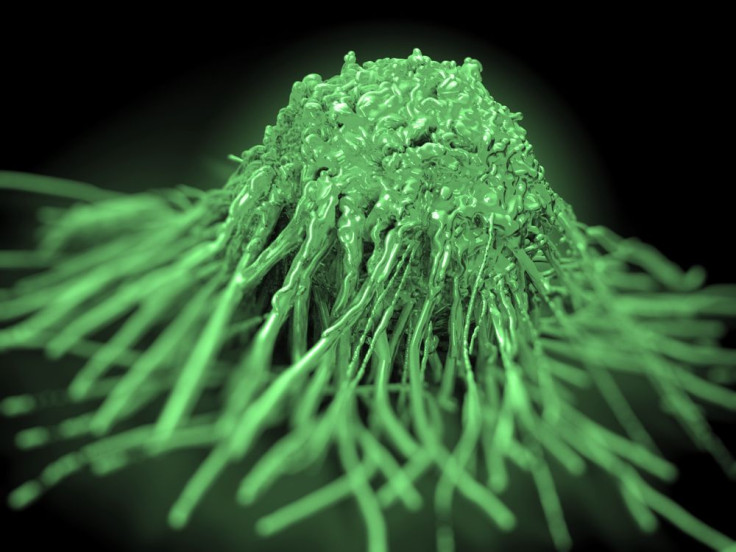
Healthy immune systems work by detecting antigens, the byproducts of bacteria, viruses, and other pathogens. Once these antigens are detected, the immune system produces antibodies to fight off and destroy the disease. Unfortunately, cancer has a way of evading the immune system. But with this form of immunotherapy, the researchers were able to use the genetically altered T cells to spot cancer and avoid evasion.
For the study, the patient’s T cells were genetically engineered to contain a receptor for a tumor antigen known as cancer-testis antigen (CT antigen), two of which are present in about 60 percent of patients with advanced myeloma. With the CT antigen receptor, the T cells were equipped to spot the myeloma and subsequently employ the immune system to find and destroy it. The results showed that 14 out of 20 patients (about 70 percent) had a near-complete or complete response three months after treatment; median progression-free survival was 91.1 months, while the overall survival lasted 32.1 months.
Although the study was small, the results are significant, study author Dr. Aaron P. Rapoport said in a press release. “The majority of patients who participated in this trial had a meaningful degree of clinical benefit. Even patients who later relapsed after achieving a complete response to treatment or didn't have a complete response had periods of disease control that I believe they would not have otherwise experienced. Some patients are still in remission after nearly three years."
Along with the impressive response to the immunotherapy treatment, no major side effects were reported in any of the patients. This suggests the treatment not only works but also poses little health risk.
There are an estimated 24,000 new cases of multiple myeloma in the United States each year. And although the cancer is treatable, it remains incurable. Currently, chemotherapy and autologous stem cell transplants remain the most popular treatment options for people with multiple myeloma. However, even with these treatments, long-term responses remain low and median survival rates range between three to five years. Rapoport says the findings represent a strong foundation for further research into the uses of cellular immunotherapy for treating multiple myeloma, with hopes of one day extending survival.
Immunotherapy has tremendous potential as a cancer treatment. Speaking to Sky News, Roy Herbst, chief of medical oncology at Yale University Cancer Center, said immunotherapy may be an “effective cure” for all cancers. His sentiment is supported by results from a June study, which investigated an immunotherapy medication as treatment for patients with advanced melanoma. Over half of the patients involved in the study saw a significant reduction in tumor size.
As scientists complete more research in this exciting field of cancer treatment, the important role of immunotherapy will likely become clearer. According to Herbst, it’s only a matter of time before immunotherapy replaces chemotherapy as the standard for cancer treatment.
Source: Rapoport AP, Stadtmauer EA, Binder-Scholl GK, et al. NY-ESO-1–specific TCR–engineered T cells mediate sustained antigen-specific antitumor effects in myeloma. Nature Medicine. 2015.



























