What Is A Concussion? The Definitive Guide For Understanding Traumatic Brain Injury

You don’t need to be on the receiving end of a Joe Frazier left hook or feel the explosive collision of one football helmet against another to suffer a concussion. They can happen just about anywhere, which means understanding how they work and what they need can predict either long-term recovery or future injury.
What’s A Concussion, Exactly?
Your brain basically sits inside a watery pile of Jell-O. In science-talk it’s called cerebrospinal fluid. This fluid acts as a cushion so that when your head gets jostled around, your brain is still able to move comfortably inside without bashing into the inner wall of the skull each time you’re headbanging to Metallica or speeding up to a red light. Still, the anatomy isn’t fool-proof.
“No matter what you put around your head, if the forces are strong enough you’re not going to prevent that brain from moving inside the skull,” Dr. Micky Collins, program director for the University of Pittsburgh Medical Concussion Program, told Medical Daily.
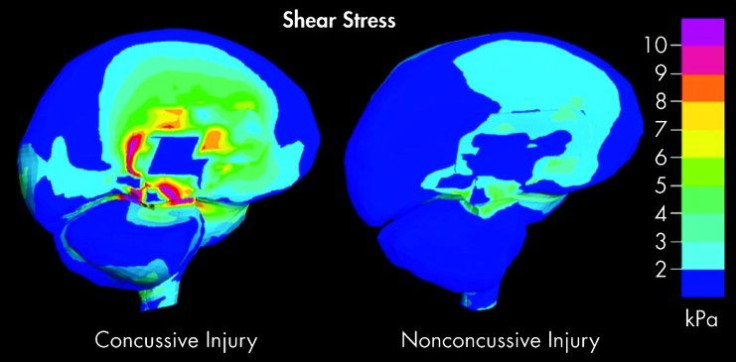
On its own, the brain sloshing around doesn’t pose much of a problem. But it’s the really hard forces that matter, because they cause damage at the cellular level. These forces cause the individual brain cells, called neurons, to stop communicating. They also cause the membranes surrounding the neurons to stretch, leaking important supplies of potassium from the cell.
“When potassium goes out of the cell,” Collins explained, “there is an increased demand for glucose — or energy, what we call ‘hyperglycolysis’ — and so the neuron is actually saying ‘Whoops, something’s wrong. I need more energy.’” At the same time, the calcium that is supposed to stay outside the cell floods the now vulnerable membrane, causing the brain to siphon off blood flow. These two conflicting forces make normal processes, such as thinking, moving, and talking, much harder. We call this resulting energy crisis a “concussion.”
Patient Recovery
Left alone, the energy crisis typically resolves itself within a few weeks. The stretched out membranes shrink back to their normal states, and cognitive processes go back to humming along like they usually do. But complications arise when patients go into their head injuries already suffering some sort of deficiency upstairs, even if it’s minor.
“Concussion fights dirty,” Collins said, referring to the injury’s knack for exploiting preexisting conditions. “Whatever system doesn’t work real well to begin with is usually what’s outed.” The research backs this up. People who suffer from migraines tend to get more migraines post-concussion; people who have eye problems keep experiencing eye problems.
Difficulties also crop up when the concussion isn’t the patient’s first. Recovery times lengthen from three weeks to as long as seven, although the good news is that full recoveries are still possible, provided patients follow-through with their physical therapy. If they don’t, that’s when the risk of long-term damage enters the picture.
The worst offense for concussion recovery is returning to play in the same sport that delivered the injury before getting the greenlight from a physician. “It’s not like adding one plus one in that situation,” Collins said. Injuries build. They compound on one another, and not always in the most noticeable of ways.
Looking Long-Term
Earlier this July, more than 4,500 retired players from the National Football League learned their lawsuit against the league was making headway. Their claim — that the NFL misled its athletes about the risks of concussion — was sound. An $870 million settlement wasn’t going to cut it.
Instead, U.S. District Judge Anita Brody ruled the NFL must stick to a formula when former players come forward seeking compensation. The formula takes into account the retiree’s condition and age. For example, a young retiree with Lou Gehrig’s disease (amyotrophic lateral sclerosis) would receive $5 million, while a retiree in his 80s would get approximately $25,000.
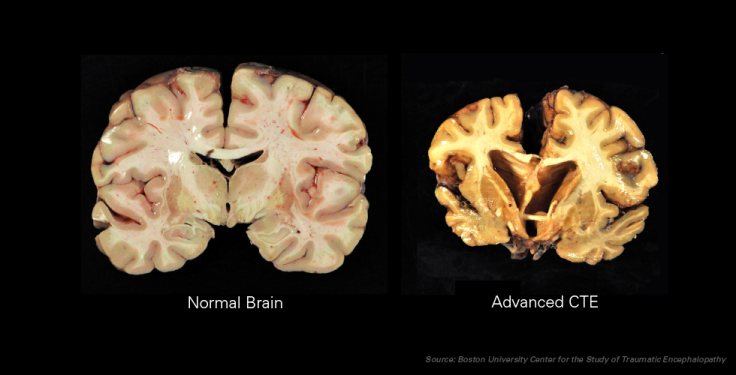
This formula, however, belies the fact that one injury stands above the rest: chronic traumatic encephalopathy, better known as CTE. First described in 2002, CTE can only be observed after death — making it a blameless non-issue for the leaders of the league but a haunting What if? for its current players. Since CTE results from hundreds, if not thousands, of sub-concussive hits, scientists can’t point to one incident alone. Of the 79 deceased athletes scientists recently opened up, 76 brains contained traces of CTE, and there isn’t a single person or thing that’s responsible.
It’s a combination of factors. Years of headfirst tackling mixed with poor medical oversight on the part of the NFL leave the hulking athletes with nothing left between their ears. They forget their names and how to perform basic functions like driving a car or getting dressed. Sometimes they suffer from other disorders simultaneously, including schizophrenia, and turn to substance abuse to numb the pain — until it ends for good.
What Comes Next
The future of concussion research comes with both good news and bad news. The good news is that scientists have the broad strokes under control. People like Collins and his colleagues can observe an injury in the brain — otherwise a locked box of information — and see a great deal of trauma without much uncertainty. This lets them design guidelines like the Heads Up program, the Centers for Disease Control and Prevention’s effort to increase awareness.
The bad news is that these programs don’t stick with people. A recent survey found the majority of parents incorrectly believed that MRI and CT scans can be used to diagnose concussion. (In actuality, the only way to diagnose concussion is with direct examination, through tests of vision, hearing, balance, and reflex.) Worse, 26 percent of parents confessed they didn’t have a firm grasp of the Return to Play guidelines, which detail how long children should wait before resuming their sport or return to school.
If there’s a silver lining in that challenge it’s that the hard problem is mostly nailed down. Generating awareness is far easier than doing the science of concussion experiments, so the better scientists can communicate with parents, coaches, and even the players themselves, the fewer concussions we’ll see.
Death rates are already falling, thanks to better equipment and safety guidelines. But incidence has jumped more than 300 cases per 100,000 since 2001. Reversing the trend means keeping a watchful eye on how we live our lives, even if Joe Frazier left hooks and colliding helmets aren’t much of a threat.



























