Female Viagra Has No 'Meaningful' Effect On Sexual Desire Disorder; Why Can't We Treat Female Dysfunction Yet?
Almost 20 years ago the Food and Drug Administration (FDA) approved Viagra, or the "little blue pill that could," as CNN called it. Men suffering from erectile dysfunction could take it to treat impotence, and in the years that followed, their choices swelled to include Levitra, Stendra, and several other performance-enhancing drugs. So how is it that pharmaceutical companies have only managed to put forth a single drug for female sexual dysfunction?
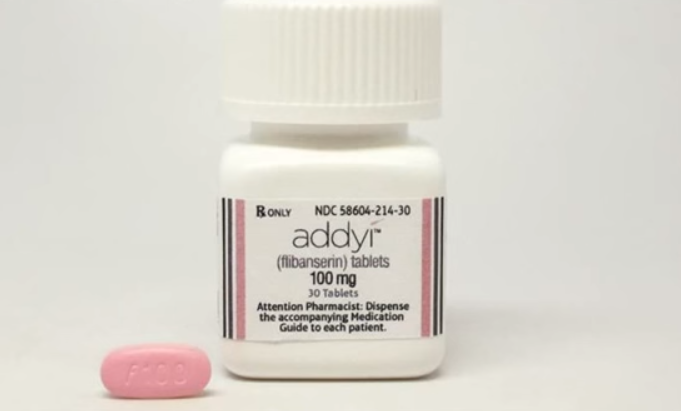
The drug is called Addyi, though many refer to it as female viagra. The FDA approved it in October 2015 for pre-menopausal women suffering from hypoactive sexual desire disorder (HSDD). By one study’s count, the disorder may occur in up to one-third of adult women in the U.S. It is marked by "a deficiency or absence of sexual fantasies and desire for sexual activity that causes marked distress or interpersonal difficulty." Women with HSDD have little interest in sex and low libido.
Like Viagra’s drug maker Pfizer, it took Sprout Pharmaceuticals, now a division of Valeant International Pharmaceuticals, years to get the FDA to sign off on the drug. But unlike Viagra it met a lukewarm response. Some experts questioned the clinical evidence that earned the drug’s approval, while others saw it as more of stepping stone or pacemaker to open the market for other drugs.
Now, seven months later, a new study published in JAMA Internal Medicine casts even more doubt on the benefits of Addyi. Researchers analyzed three trial registries and 13 electronic databases, including Embase.com, Medline, and Psycinfo, for studies assessing the drug’s efficacy and safety. Eligible studies included measures for how Addyi affected women’s sexual interest and arousal disorder, as well as any side effects, from a change in the number of satisfying sexual events to dizziness, nausea, and fatigue. Women were either taking Addyi or a placebo.
Two independent researchers reviewed all abstracts and trials and graded their evidence using a system developed to establish whether study recommendations are strong, weak, or biased.
In the end, only eight of the researchers' results were even eligible for reviews and grades; five published and three unpublished studies involving around 6,000 women. They found the overall quality of the evidence and safety outcomes was very low. But on average, women on Addyi had one-half of an additional satisfying sexual event over those not on the drug while experiencing more dizziness, sleepiness, nausea, and fatigue. And those side effects may increase with alcohol consumption and oral contraceptive use.
Researchers concluded that the meaningful benefit between women taking Addyi and a placebo "was small, ranging from minimal improvement to no change." That said, they admitted their analysis was limited in that the data they collected was "light on details." More importantly, it was not a diverse sample of women; all participants were in a stable, heterosexual, and monogamous relationship for at least a year. These findings are hard to generalize when they leave out women who may be in a non-monogamous relationship; taking additional medication; or struggling with other mental health issues, like depression.
"With nearly 90 percent of American physicians indicating that they would prescribe an approved HSDD pharmacological product over available non-pharmacological treatments, the need for sound evidence on the efficacy and safety profile of Addyi is evident," researchers said. "It has been suggested that women with HSDD would benefit most from an integrative approach, including medical, psychiatric, psychological, couple-relation, and socio-cultural domains."
Quality, not quantity
The gender disparity in the marketplace may be fueled by the ways we talk about female sexual dysfunction. The conversation can’t just be about how much sex women are having, it has to be about the quality of these encounters, too. In an interview with Mother Jones about Addyi, sex educator and author of Come As You Are Emily Nagoski pointed out that its purpose was to "create desire." And yet, she said, "the point of desire falls flat if women aren’t experiencing pleasure."
Addyi works by increasing the levels of hormones dopamine and norepinephrine at the same time as it decreases levels of serotonin. The former two are thought to increase sexual desire while the latter is thought to decrease it. But this banks on the idea that women’s sexual desire is a result of something physiological, when in fact, a 2003 study from the Kinsey Institute found predictors of sexual distress in women were more psychological.
After interviewing 987 women about their sexual experiences over the phone, Kinsey researchers found that physical aspects of sexual response, including arousal, vaginal lubrication, and orgasm, were poor predictors of disorder. Instead, the best predictors had to do with women’s mental health, which researchers intuited based on answers to questions about "feeling calm and peaceful, having lots of energy, feeling downhearted and blue, and having work and other functions impaired by emotional problems."
It is possible that sexual distress put women in a negative mental state; however, researchers said that, given the number of women who reported experiencing depression, "it is likely that in the majority of our cases it was the negative mental state that led to the sexual distress rather than the other way round." Overall, they concluded that the "lack of emotional wellbeing and negative emotional feelings during sex were more important determinants compared to physiological aspects of female sexual response."
HSDD clearly manifests itself differently in men and women, so it doesn’t make sense to develop female equivalents of male drugs. Without a specific approach to assess women with the disorder, the gender disparity will remain.
More importantly, if women’s low sexual desire is prompted by psychological stressors, be it a lack of partner communication or depression, then that would need to be added to the conversation; the solution is not always physical. Drugs will not work in either men or women if the root cause of the problem goes untreated.
Source: Jaspers L, Franco OH, et al. Efficacy and Safety of Flibanserin for the Treatment of Hypoactive Sexual Desire Disorder in Women: A Systematic Review and Meta-Analysis. JAMA Internal Medicine. 2016.



























