Antibiotic-Resistant Bacteria Can't Handle Attacks From Engineered Enzymes 'Programmed' To Target Them
For years, doctors have warned about the dangers of overusing antibiotics. They're powerful antibacterials capable of flushing out disease-causing germs, but in the process they also endanger the good bacteria present in our bodies. But what's more, misusing antibiotics can also build up resistance in pathogenic bacteria, causing the antibiotics to fail, and previously managed diseases to be untreatable.
Now, researchers from the Rockefeller University in New York City have developed an antibiotic that can be "programmed" to selectively target pathogenic bacteria, specifically those that develop resistance, while leaving other bacteria untouched. The paper will be published on Sunday in the journal Nature Biotechnology.
"In experiments, we succeeded in instructing a bacterial enzyme, known as Cas9, to target a particular DNA sequence and cut it up," said lead researcher Luciano Marraffini, head of the university's Laboratory of Bacteriology, in a statement. "This selective approach leaves the healthy microbial community intact, and our experiments suggest that by doing so you can keep resistance in check and so prevent certain types of secondary infections, eliminating two serious hazards associated with treatment by classical antibiotics."
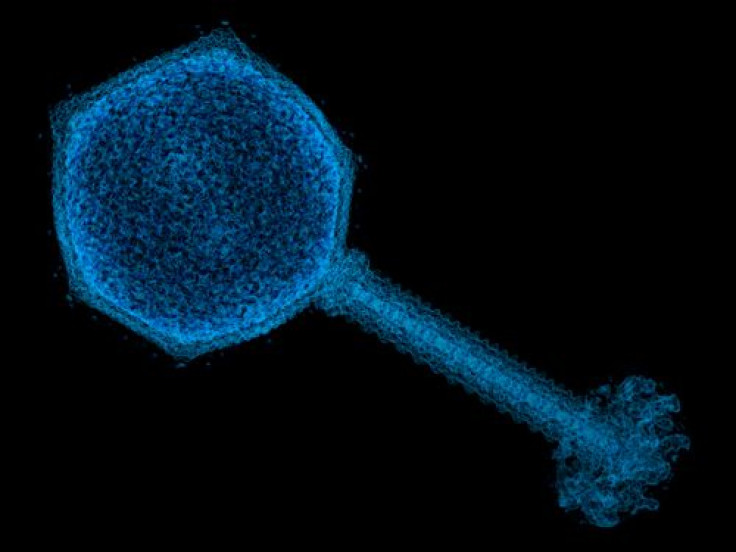
The enzyme, Cas9, is part of bacteria's defense systems against invading viruses. As part of the CRISPR-Cas (clustered regularly short palindromic repeats), it uses unique genetic sequences called spacers, which correspond to sequences on viruses. Cas9 and its related enzymes use these spacers as guides to identify and fight viral invaders.
The researchers were able to modify Cas9 to use it against specific microbes. They did this by engineering the enzyme's spacer sequences to match the genes of the bacteria they were targeting, and then inserted them into a cell along with the Cas9 gene. When the cell became active, it could match up with the bacteria it was engineered for, and Cas9 would either kill the bacteria or eradicate the target gene. The researchers even found that this treatment prevented some cells from acquiring resistance.
"We previously showed that if Cas9 is programmed with a target from a bacterial genome, it will kill the bacteria. Building on that work, we selected guide sequences that enabled us to selectively kill a particular strain of microbe from within a mixed population," first author of the study David Bikard said in the release.
The scientists were able to demonstrate effectiveness of the antibiotic against Staphylococcus aureus, a common bacterium of the skin and respiratory tract responsible for several diseases. The scientists used strains of S. aureus that had become resistant to kanamycin. Their engineered antibiotic killed most of the bacteria, while leaving behind those that were still susceptible to kanamycin.
But would this work against more "intelligent" bacteria, which share antibiotic-resistant genes among themselves, rapidly developing resistance? The researchers knew that for the antibiotic to be effective it would have to target the part of the bacteria's DNA that spreads the antibiotic-resistant gene: the plasmid.
To test this, the scientists let Cas9 loose on tetracycline resistant-harboring plasmids in multidrug-resistant S.aureus (MRSA), a strain that's especially strong and potentially deadly. Not only did Cas9 destroy the plasmids and make the resistant cells sensitive to tetracycline, but it also prevented other S. aureus cells from becoming antibiotic resistant.
These experiments were also tested on the skin of live mice, which showed that the antibiotic could effectively kill kanamycin-resistant S. aureus causing infection on their shaved backs. Though the treatment may be successful, the scientists said they need to work on how the antibiotic is delivered. The current mode involved injecting the Cas9 enzymes into the bacterial cells. The scientists hope to find a broader way of delivering it so that it can fight other infections, such as colon infections caused by Clostridium difficile.
Source: Marraffini L, Bikard D, et al. Nature Biotechnology. 2014.



























