New 3D-Imaging Technique Reveals How Pulmonary Fibrosis Develops
A weary patient with a dry, hacking cough appears in the waiting room of her doctor’s office. During the examination, she reports aches and pains; each breath, she says, is increasingly difficult to take. The doctor makes a note on his clipboard, and avoids the patient’s steady brown eyes. Later, X-rays and CT scans reveal the tissue in her lungs has become inflamed, while some has even thickened and stiffened into scars. The diagnosis: idiopathic pulmonary fibrosis. The prognosis: three to five years left to live.
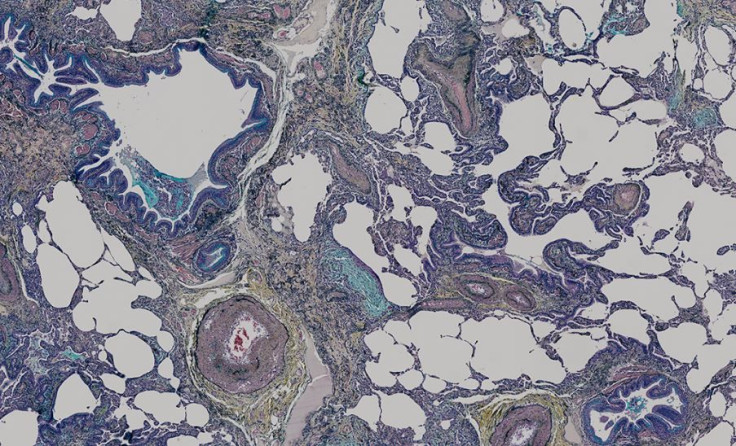
Previously, scientists believed the scarring progressed like a wave from the outside to the inside of the lung. Instead, a new study finds a large number of individual sites within the lungs undergo active disease scarring. To make this discovery, the Southampton Respiratory Biomedical researchers used advanced 3D X-ray imaging technology originally designed for the analysis of engineering parts, such as jet turbine blades. Insights gained from this powerful scanning equipment should help scientists develop targeted therapies focusing on these areas, the researchers said.
“Idiopathic” is a word doctors use when they do not know the cause of a condition or disease. Idiopathic pulmonary fibrosis or IPF is one of a group of disorders known collectively as interstitial lung diseases. Though IPF usually affects middle-aged and older adults, the disease varies from person to person. In some, the disease is aggressive, appearing suddenly and reducing a person’s life to a handful of remaining years. In others, the process is much slower and the disease remains unchanged for years. The overwhelming majority of cases are singular, happening once in a family, and only a small percentage of people have another family member with the disease. Scientists do not yet understand how genetics influence the condition.
For the study, lead author Dr. Mark Jones and his colleagues examined lung biopsy specimens from four patients, diagnosed by expert pulmonary pathologists. The researchers then processed and embedded the samples in paraffin wax. After using an integrated microfocus CT scan to view the specimens, the researchers reconstructed the projections in 3D. The microfocus CT scan allowed them to accomplish this by taking thousands of 2D images of the specim, all while slowly rotating it 360 degrees.
What they discovered surprised many scientists familiar with the disease. Within each tissue sample, Jones and his colleagues saw numerous, complex fibroblasts that varied in their shape and volume. Fibroblasts are cells that synthesize collagen and proliferate in pulmonary fibrosis, contributing to the thickening of lung tissue. Unexpectedly, however, each fibroblast was an independent structure with no connections to other fibroblasts.
This led the researchers to conclude that IPF is more an accumulation of individual diseased cells than a wave. The Southampton team is now studying how they might use their technology and technique with similar diseases, to help doctors improve diagnosis and treatment.
Source: Jones MG, Fabre A, Schneider P, et al. Three-dimensional characterization of fibroblast foci in idiopathic pulmonary fibrosis. JCI Insight. 2016.
Published by Medicaldaily.com



























