Drinking While Pregnant: More Than 3 Million Women At Risk Of Exposing Baby To Alcohol During Early Stages Of Pregnancy

Too many women are in danger of inadvertently drinking alcohol during the early stages of pregnancy, according to new research published Tuesday by the Centers for Disease Control and Prevention (CDC).
Analyzing two years' worth of data from a nationally representative survey, the authors estimated that approximately 3.3 million women were at risk of an alcohol-exposed pregnancy during the past month, defined as having unprotected sex with a fertile partner while still regularly consuming alcohol. Overall, 7.3 percent of women from the ages of 15 to 44 were found to be at risk of early alcohol exposure during a potential pregnancy, and even among women who explicitly went off contraception in order to conceive, three-fourths continued to drink.
“Alcohol can permanently harm a developing baby before a woman knows she is pregnant,” said Dr. Anne Schuchat, CDC Principal Deputy Director, in a statement. “About half of all pregnancies in the United States are unplanned, and even if planned, most women won’t know they are pregnant for the first month or so, when they might still be drinking. The risk is real. Why take the chance?”
The authors used data from the National Survey of Family Growth (2011-2013), ultimately focusing on 4,303 nonpregnant, nonsterile women. In particular, they found the greater risk was seen in married women over single women (11.7 percent vs 2.3 percent), smokers over nonsmokers (10.7 percent vs 6 percent), and women who already had a prior pregnancy over those who hadn’t (13.6 percent vs 5.8 percent). Sexually active teen women were among the least likely to be exposed to alcohol (2.2 percent).
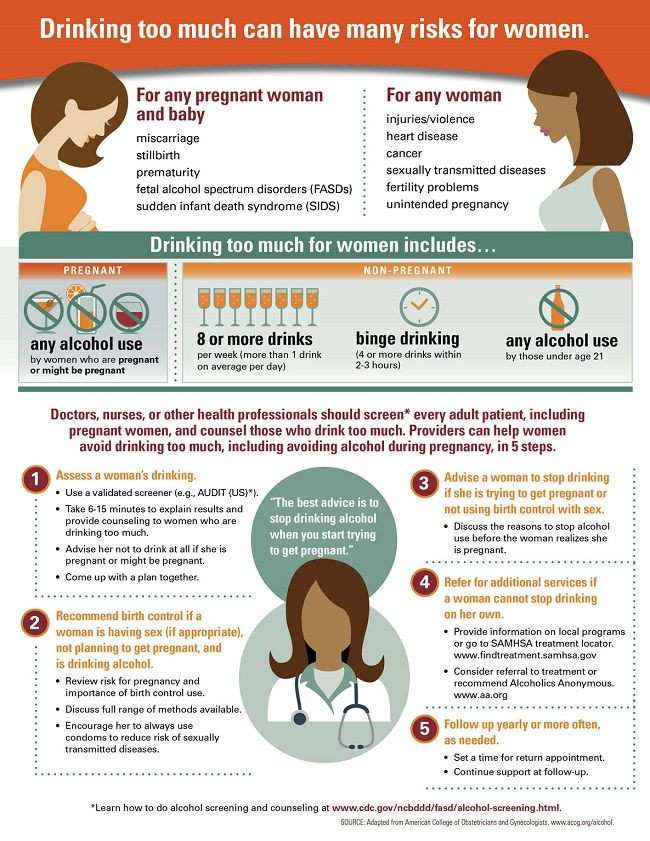
“Every woman who is pregnant or trying to get pregnant — and her partner — want a healthy baby. But they may not be aware that drinking any alcohol at any stage of pregnancy can cause a range of disabilities for their child,” said Dr. Coleen Boyle, director of CDC’s National Center on Birth Defects and Developmental Disabilities. “It is critical for healthcare providers to assess a woman’s drinking habits during routine medical visits; advise her not to drink at all if she is pregnant, trying to get pregnant or sexually active and not using birth control; and recommend services if she needs help to stop drinking.”
Boyle’s declaration on the absolute harms of alcohol use during pregnancy, though echoed by organizations such as the American Academy of Pediatrics, isn’t as concrete as it appears. While binge drinking is widely acknowledged to place a fetus at risk of developmental disorders, the research on whether light drinking (typically less than a glass per day), poses a similar danger is mixed. Some, such as Emily Oster, an Associate Professor of Economics at Brown University and author of Expecting Better: Why the Conventional Pregnancy Wisdom Is Wrong, have argued the data doesn’t support an universal ban on alcohol, though the occasional drink should likely be postponed until later trimesters.
Even if light drinking is safe for expectant mothers, though, that doesn’t preclude the importance of reaching out to women who could soon become pregnant and educating them about the broader risks of drinking alcohol, nor of providing them the means to better manage their varying lifestyle habits and needs, especially in light of prior CDC research showing that only one in six adults actively talk about their alcohol use with their doctors.
“To help prevent adverse consequences of alcohol consumption during pregnancy, health care providers should discuss and recommend, as appropriate, available contraception methods, including condoms to protect against sexually transmitted diseases, to women who are sexually active and drink alcohol,” the CDC authors wrote.
Source: Green P, McKnight-Eily L, Tan C, et al. Vital Signs: Alcohol-Exposed Pregnancies — United States, 2011–2013. MMWR. 2016
Published by Medicaldaily.com



























